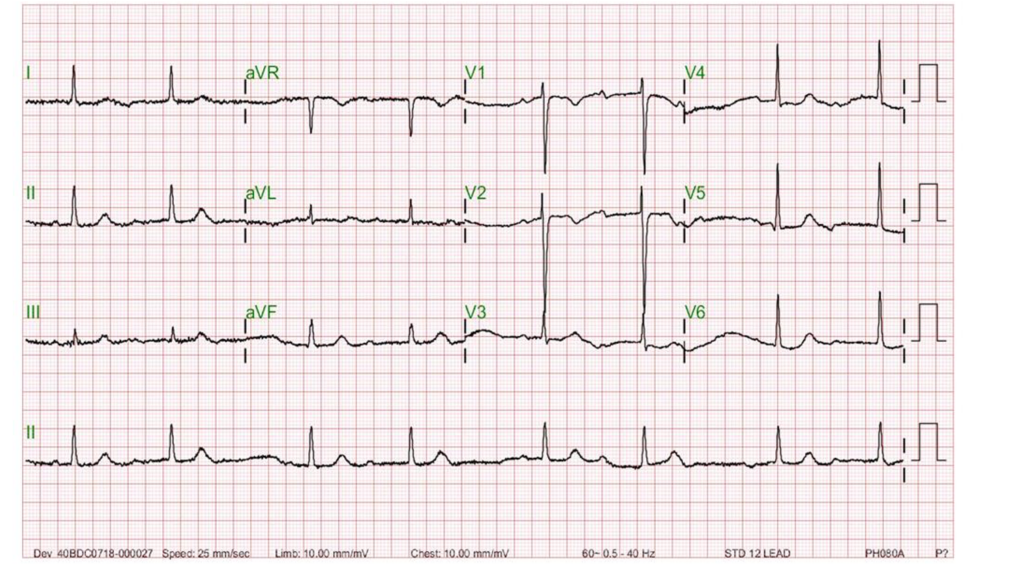
Case 30

This 86-year-old woman with a long-standing history of hypertension, COPD, anemia, and hypertrophic obstructive cardiomyopathy (HOCM) was brought to the emergency department complaining of SOB associated with general malaise and productive cough with yellowish sputum for one week.
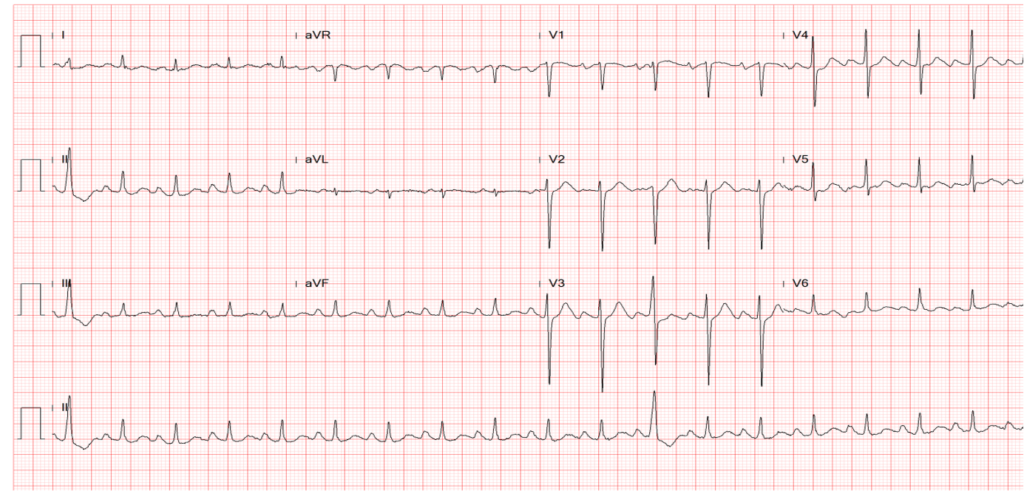
Case 29
A 56-year-old man came to the Emergency Department because of worsening dyspnea with a productive cough for the past two weeks. Notably, he smoked one pack of cigarettes a day and had COPD with bronchiectasis for more than 20 years.
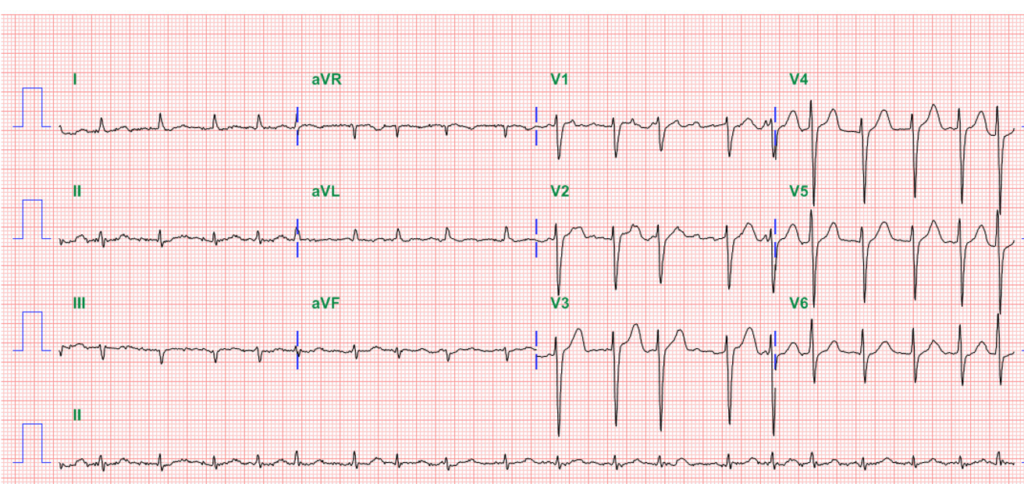
Case 28
This 92-year-old man complained of progressive dyspnea with PND, productive cough with whitish sputum, and bilateral leg edema for the past few weeks. He was a poor historian. Except for COPD, he recalled diabetes mellitus (DM) disclosed by a local physician two weeks prior. At the Emergency Room, he appeared apprehensive and was in moderate respiratory distress.
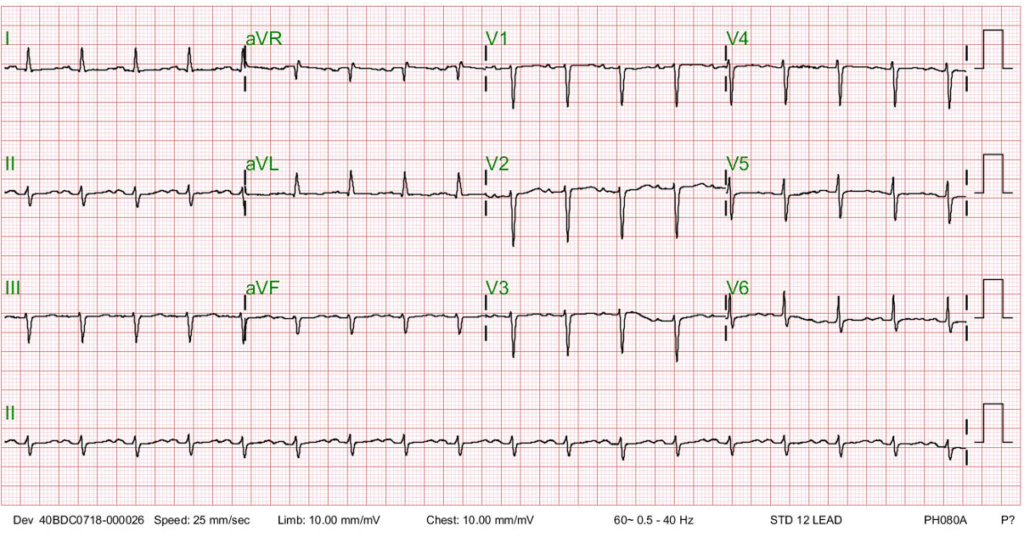
Case 27
This 50-year-old man came to the Emergency Department complaining of having substernal chest pain for more than 10 hours. The pain was sharp and not exertion-related. It could radiate to the left shoulder, back, and scapula. It seemed positional, as inspiration could worsen it, and leaning forward could somewhat mitigate the pain. At times, he also experienced nausea, dyspnea, and cold sweats. Reportedly, he had flu-like symptoms with a runny nose and sore throat but didn’t visit any clinic seeking help. Past medical history was significant for thalassemia, mild GERD, and gallbladder stone diagnosed ten years ago.
Case 26

This 50-year-old man came to the Emergency Department complaining of having substernal chest pain for more than 10 hours. The pain was sharp and not exertion-related. It could radiate to the left shoulder, back, and scapula. It seemed positional, as inspiration could worsen it, and leaning forward could somewhat mitigate the pain. At times, he also experienced nausea, dyspnea, and cold sweats. Reportedly, he had flu-like symptoms with a runny nose and sore throat but didn’t visit any clinic seeking help. Past medical history was significant for thalassemia, mild GERD, and gallbladder stone diagnosed ten years ago.
Case 25
This 75-year-old man came to the Emergency Department (ED) complaining of abdominal pain for one day. He claimed he had constipation for several months, for which he took a laxative daily. He also noticed muscle weakness, especially in the lower extremities, which he accounted for his falls while climbing a staircase and riding a bike within the past five days.
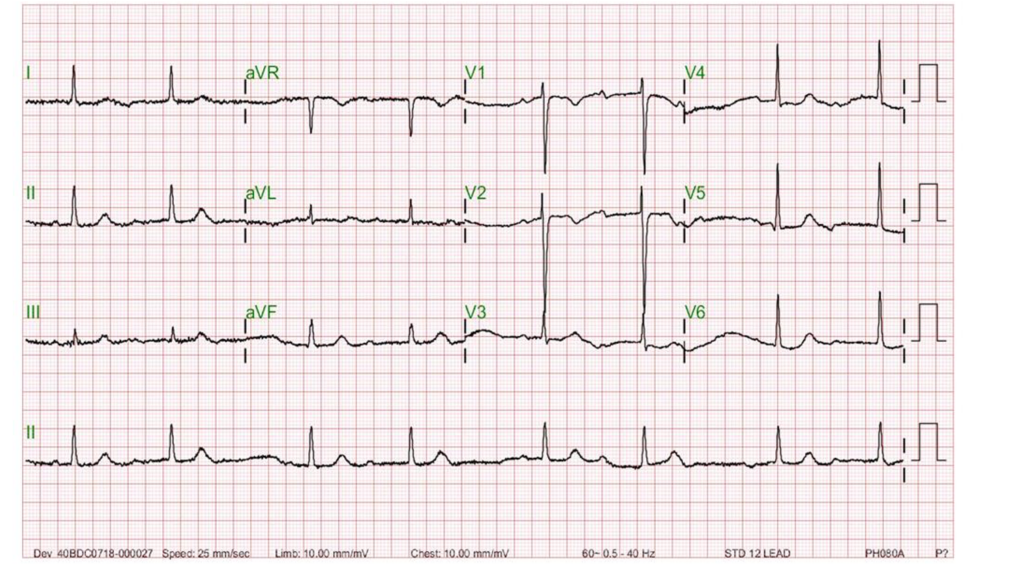
Case 24
An 88-year-old woman complained of a loss of appetite, generalized weakness for two weeks, and increasing SOB for five days. She had chronic heart failure (HF), presumably caused by hypertension and diabetes mellitus, for over 30 years. She also had chronic renal dysfunction complicated by anemia.
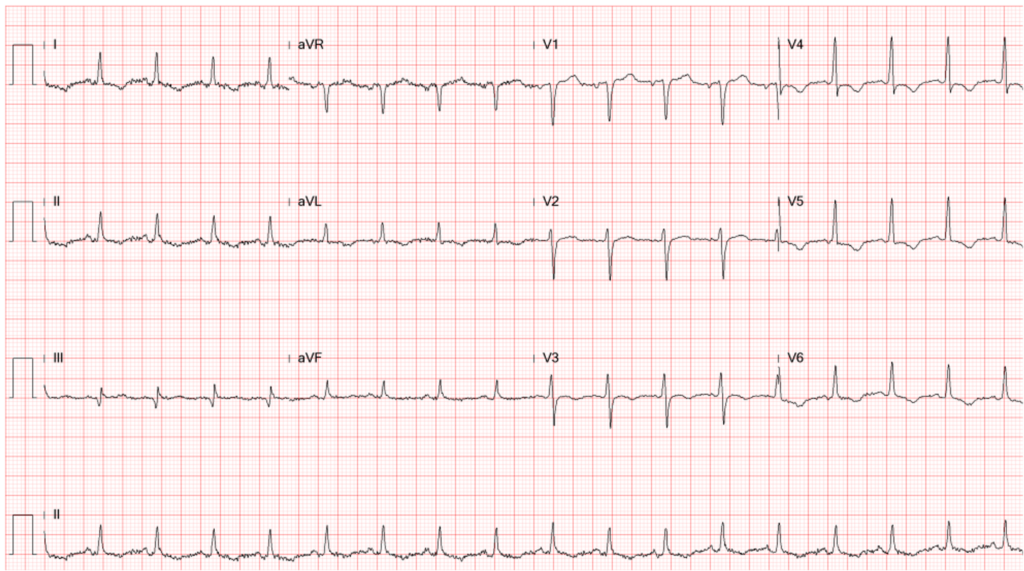
Case 23
This 72-year-old man, a retired coal miner with a known history of chronic obstructive pulmonary disease (COPD) and pneumoconiosis, came to the Emergency Department complaining of increasing SOB for two days.
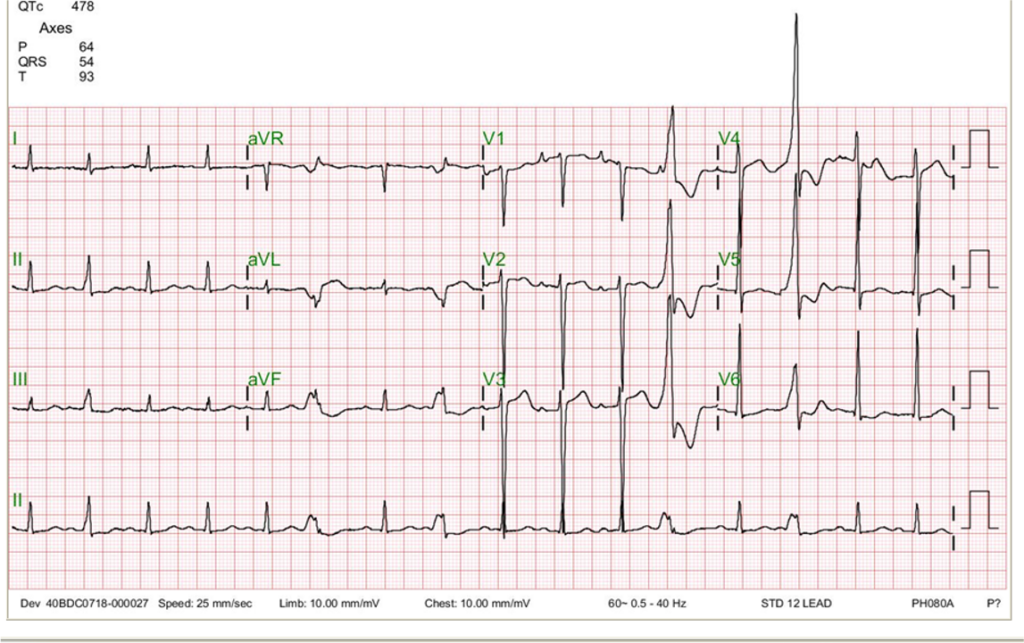
Case 22
An 84-year-old man with a known history of hypertension, COPD, diabetes, Parkinsonism, and old CVA (putamen infarction)* was noted to be delirious after five days of having reduced appetite and general weakness.
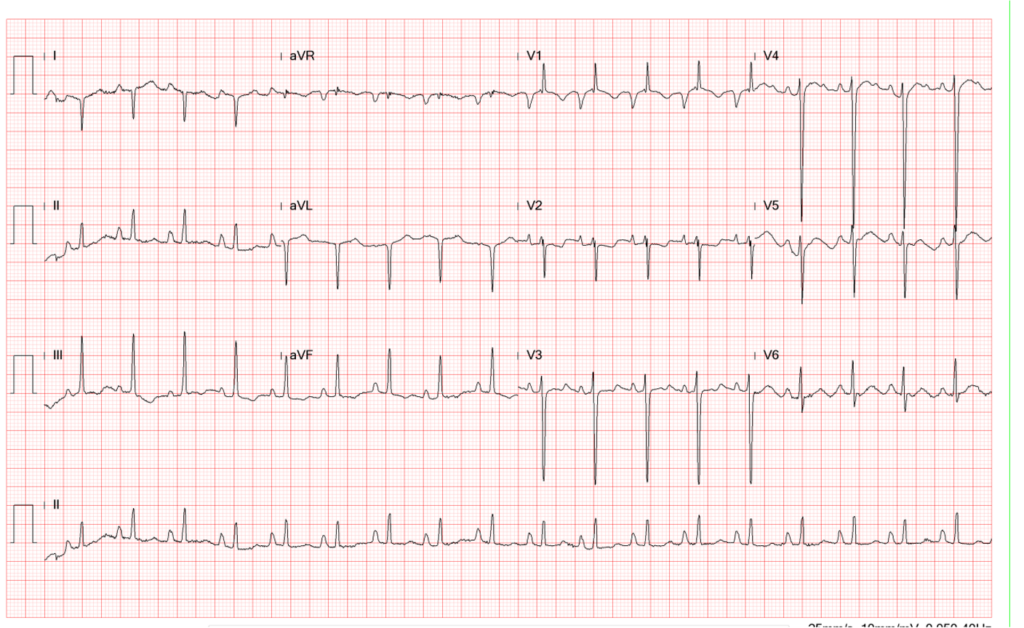
Case 21
A 41-year-old Taiwanese woman, G3P1, developed progressive dyspnea on exertion, PND, and orthopnea for five days after she gave birth to a healthy baby boy (vaginal delivery) three months prior.