Case 34

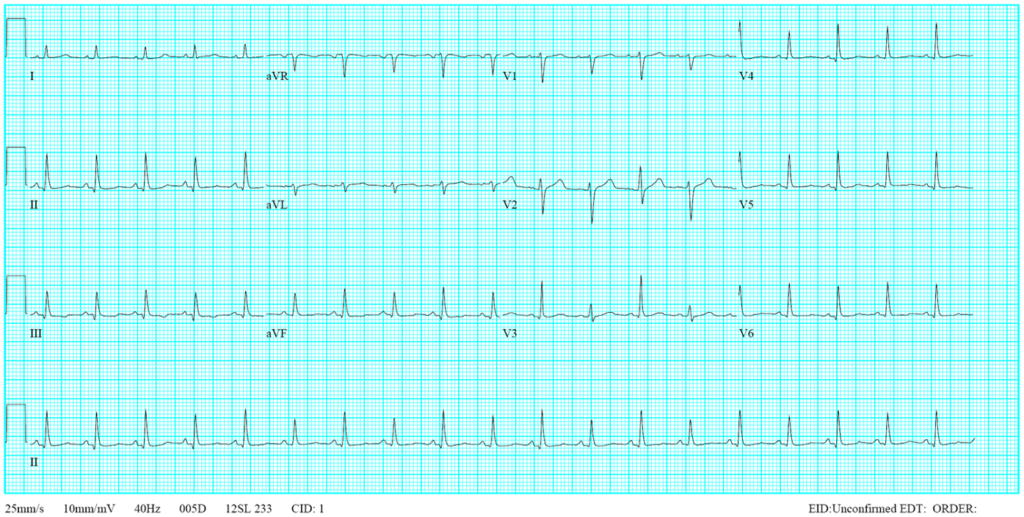
Case 34 Content When this 78-year-old man walked into t […]
Case 33
This 35-year-old male was transferred from a local hospital for further evaluation after a biopsy of a hard, 4 cm in diameter lymph node in the left supraclavicular fossa (Virchow’s node)* suggestive of metastatic malignancy. His chief complaint was progressive SOB with a productive cough for the past week despite having received rifampicin and ethambutol therapy for recently diagnosed pulmonary tuberculosis (TB) for about one month. He claimed to have lost 8 kg in the past six months.
Case 32
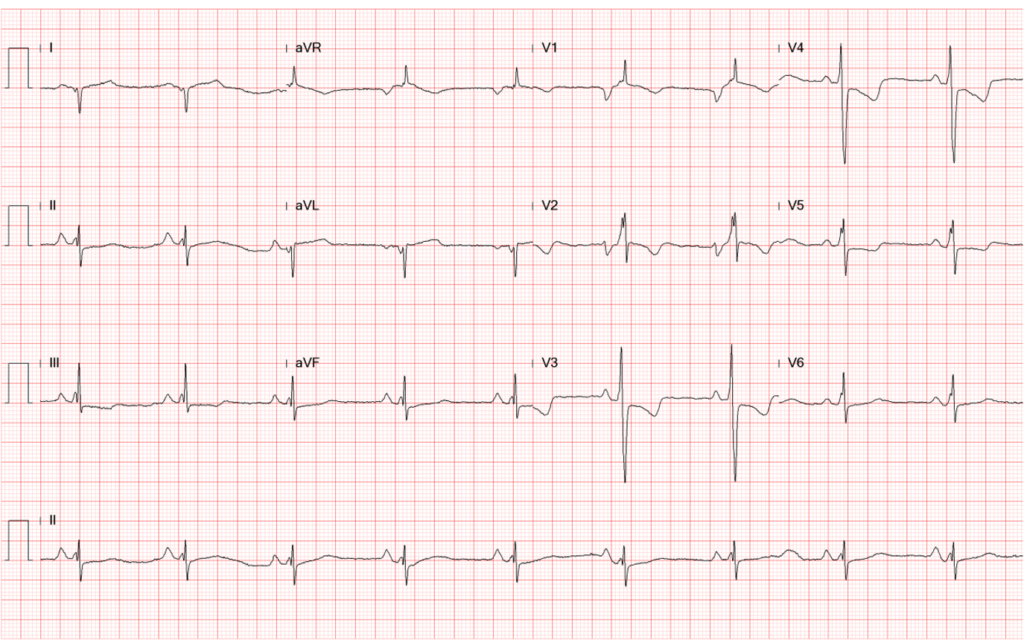
A 52-year-old man was admitted because of progressive dyspnea on exertion for one week. In the past, he had chronic obstructive pulmonary disease (COPD), alcoholic liver cirrhosis with minimal esophageal varices, gastroesophageal reflux, and duodenal ulcer with bleeding but no hypertension, diabetes mellitus, or atherosclerotic coronary heart disease (CHD). He was one pack a day smoker and a daily drinker for at least 25 years.
Case 31
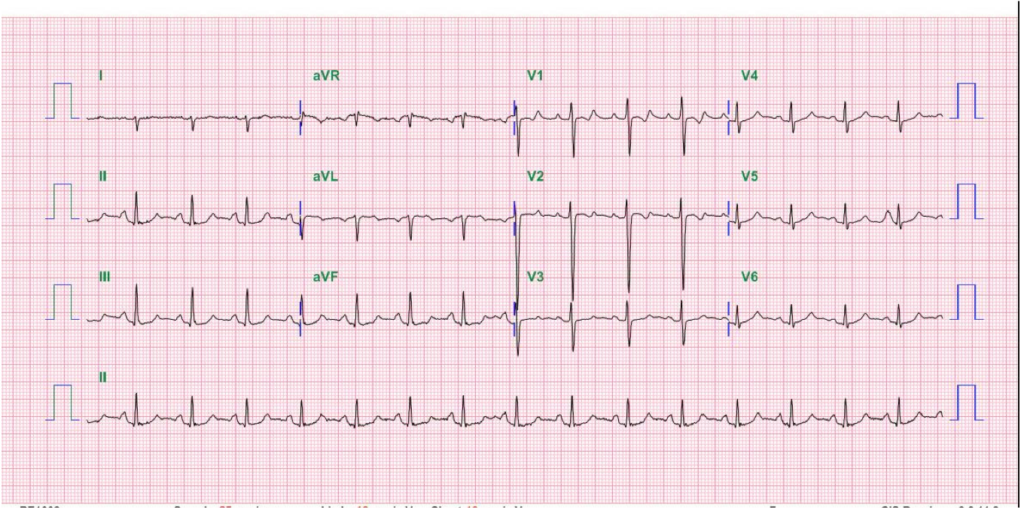
A 41-year-old man with Limb-Girdle muscular dystrophy (LGMD) was brought to the Emergency Department complaining of having intermittent chest tightness, cold sweating, and shortness of breath (SOB) for one day and a near syncope episode two hours prior. Past medical history is significant for hypertension and chronic hepatitis B for a few years and an uneventful PTCA with stenting for left anterior descending artery (LAD) stenosis (single vessel coronary heart disease) presenting as non-ST elevation myocardial infarction (NSTEMI) two months before.