
Case 24
An 88-year-old woman complained of a loss of appetite, generalized weakness for two weeks, and increasing SOB for five days. She had chronic heart failure
The 56-year-old man came to the Emergency Department complaining of progressive dyspnea and chest tightness with a nonproductive cough for six months despite a few weeks of antibiotic treatment. He also described having low-grade fever and night sweats but no diarrhea, dysuria, PND, or orthopnea. Past medical history was significant for diabetes mellitus (DM) and hypertension, for which he had been taking anti-DM and antihypertensive medications for over ten years. He appeared chronically ill and was in moderate respiratory distress. BT/PR/RR was 36.7 ºC/108/min/19/min, and BP measured 134/86 mmHg. JVD was 10 cm H2O, and the liver was 3fb palpable below the right costal margin. PMI was not visible, heart sounds were distant, but no murmurs were audible. ECG showed diffuse low voltage and sinus tachycardia at 103/min with T wave inversion in leads I, II, aVL, and V3-V6. Chest X-ray exhibited a marked increase in the silhouette, suggesting cardiomegaly, a small right pleural effusion, and hepatomegaly. Pertinent laboratory data included Hb 10.4 g/dL, HCT 30.3 %, WBC 9990 (Neutrophil 76.6 %), CRP 4.5 mg/dL, Glu 204 mg/dL, Plt 439 K/ul, BUN 17 mg/dL, Cr 1.03 mg/dL, Na 136 mEq/L, K. 3.6 mEq/L, SGOT 61 U/L, GPT 121 U/L, GGT 58 U/L, TBil 1.82 mg/dl, ALP 106 U/L, INR 1.26, PT 13.5 sec, aPTT 30.4 sec, troponin I 0.02 ng/ml, CKMB 0.02 ng/ml. Subsequent echocardiography revealed significant pericardial effusion. Abdominal echo revealed fatty liver, a hepatic tumor, likely hemangioma, and gallbladder sludge. The CT scan confirmed massive pericardial effusion and right-side pleural effusion as well; there was no tumor or lymphadenopathy. Accordingly, the care team did pericardiocentesis, removed 533 ml of reddish fluid, and inserted a pigtail for drainage. The pericardial fluid appeared exudate containing protein 4.7 gm/dL (serum protein 5.6g/dl) and LDH 1393 U/L (serum LDH 360 U/L) without identifiable organisms under the microscope. The pigtail drained out 70-200 ml of pericardial fluid daily, while daily care documented intermittent low-grade fever (37.8-38.8 ºC). Following consultation with the cardiovascular specialist, a surgeon performed a partial pericardiectomy. The pericardial biopsy revealed granulomatous inflammation with caseous necrosis and was positive for the acid-fast bacillus (AFB) stain, tuberculosis polymerase chain reaction (PCR), and adenosine deaminase (ADA) (+)*. Under the diagnosis of TB pericarditis, The care team added IV steroid (solu-medrol), along with a combination anti-TB chemotherapy (Rifater/Rifinah)** aiming at further reducing the inflammation of the pericardium and improving the survival rate (not proven effective strategy). They also added rapamycin to co-trimoxazole for status post pericardiectomy and possible secondary lung infection. Three weeks later, his liver dysfunction resolved, as TBil, ALK, GOT, GPT, and GGT all returned to normal ranges, and the patient’s condition significantly improved.
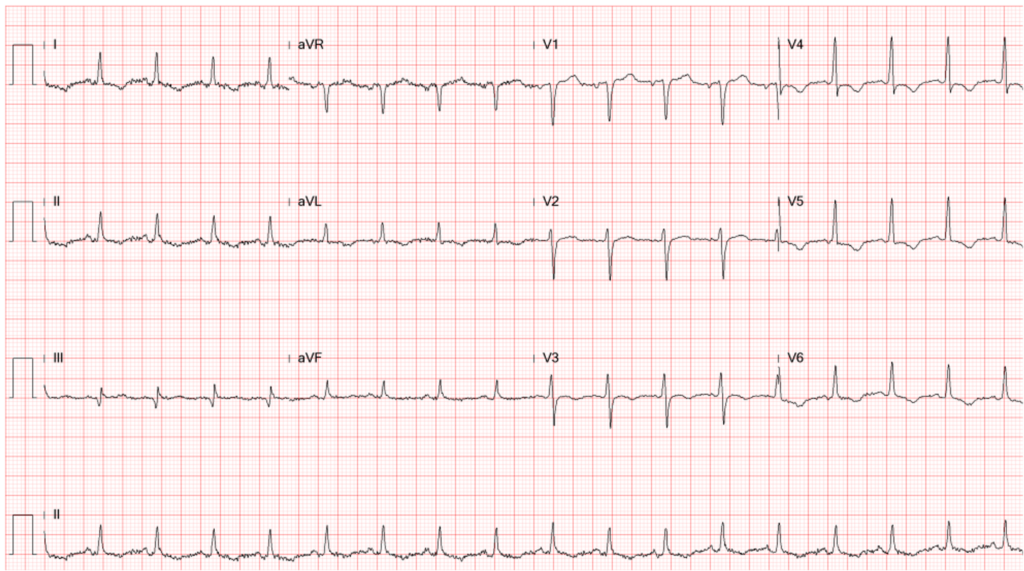
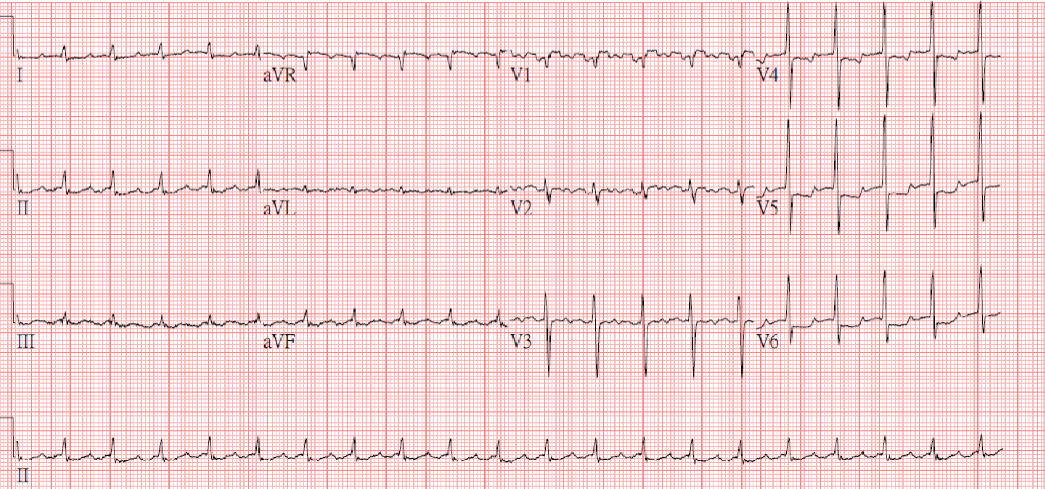
Diffuse low voltage
Sinus tachycardia at 103/min
Nonspecific ST-T changes with T wave inversion in leads I, II, aVL, and V3-V6

A marked increase in the cardiothoracic ratio suggestive of cardiomegaly.
Small aortic knob
Blunting of right costophrenic angle consistent with pleural effusion
Minor fissures discernible (r/o mild HF)
Hepatomegaly

A marked decrease in the cardiothoracic ratio after pericardiocentesis.
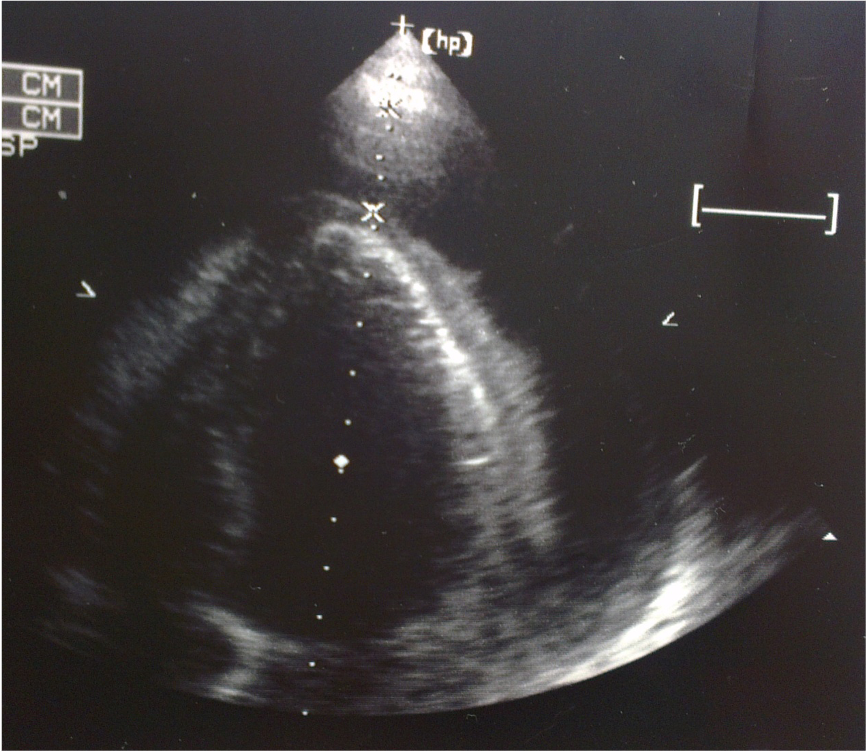
Pericardial effusion as indicated by arrow
Insertion of a pigtail into the pericardial space for drainage

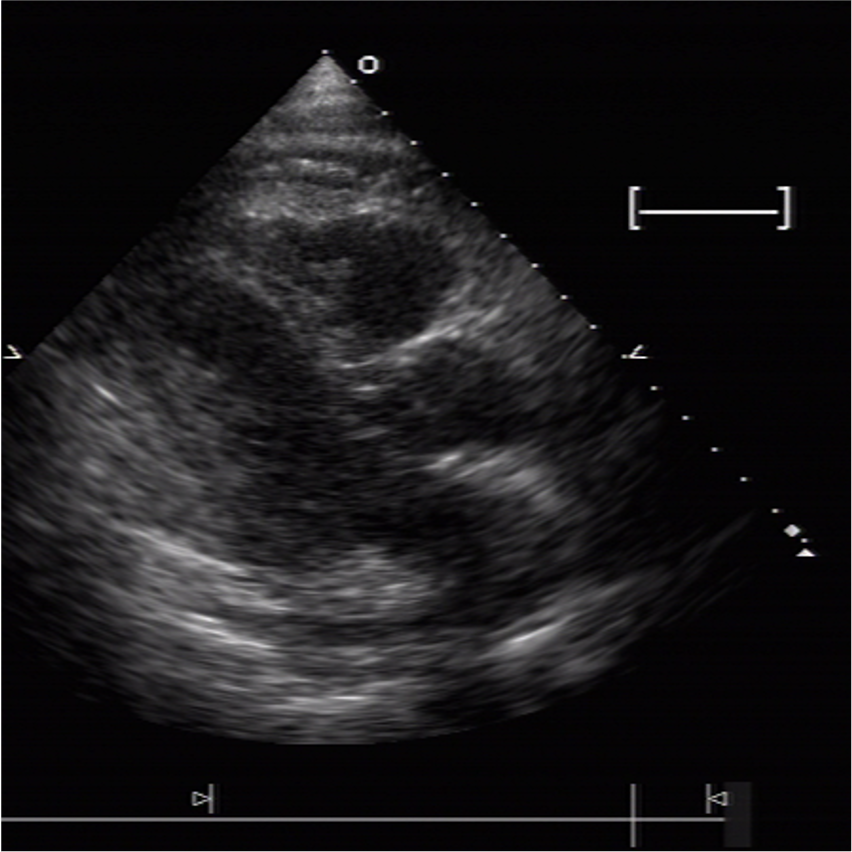
Massive pericardial effusion, as indicated by an arrow
Right side pleural effusion
No tumor or lymphadenopathy
Typical ECG changes due to acute pericarditis include widespread concave ST elevation and PR depression throughout most limb leads (I, II, III, aVL, aVF) and precordial leads (V2-V6), reciprocal ST depression and PR elevation in lead aVR (± V1) and sinus tachycardia. However, these ECG features may not be seen in tuberculosis pericarditis with effusion. In the present case, the ECG showed diffuse low voltage and sinus tachycardia with T wave inversion in leads I, II, aVL, and V3-V6. With a significant amount of pericardial effusion (> 500 ml), ECG shows diffuse low voltage but no electrical alternans,*** another additional feature that might be associated with pericardial effusion.
Tuberculosis pericarditis is a form of pericarditis caused by Mycobacterium tuberculosis, the same bacteria that causes tuberculosis (TB) in the lungs. It may occur via extension of infection from the lung or tracheobronchial tree, adjacent lymph nodes, spine, sternum, or via miliary spread. Unfortunately, in many patients, the primary focus of pericardial infection remains elusive. Nevertheless, it is a severe condition, as it can lead to fluid accumulation in the pericardial space, causing symptoms such as chest pain, shortness of breath, and fatigue. Clinically, it may not be easy to diagnose. If the diagnosis is missed or delayed, it can result in late complications such as constrictive pericarditis, thereby increasing mortality. Diagnosing tuberculosis pericarditis requires careful clinical assessment, imaging studies such as chest X-ray, echocardiography, chest CT scan, and laboratory tests, including pericardial fluid analysis, tissue biopsy, and tuberculosis testing, as demonstrated in the present case.
As noted in the present case, the Chest X-ray may show an enlarged cardiac silhouette, suggesting cardiomegaly. However, echocardiography and chest CT scan revealed the presence of a large amount of pericardial effusion. Echocardiography is also helpful in identifying RA and RV collapse during diastole and dilated inferior vena cava (IVC), hallmark findings of cardiac tamponade, which is a medical emergency. Besides, echocardiography can guide the performance of pericardiocentesis while draining the pericardial fluid. It helps visualize the needle insertion site, monitor the drainage process, and assess the effectiveness of fluid removal. Laboratory tests play a critical role in the diagnosis of tuberculosis pericarditis. These include: 1. Tuberculin skin test (TST) with purified protein derivative (PPD) from the bacteria. 2. Interferon-gamma release assays (IGRAs) for exposure to the bacteria (antigen): positive TST and positive IGRA indicate exposure to tuberculosis. Still, they do not differentiate between active and latent infection. 3. Pericardial fluid analysis through pericardiocentesis; the fluid is analyzed for the presence of Mycobacterium tuberculosis using various tests, including AFB stain, ADA, culture, and PCR. as shown in the present case.
Management of tuberculosis pericarditis depends on the presence or absence of effusion. When the effusion is large, it may cause cardiac tamponade, and pericardiocentesis is mandatory to relieve symptoms like the present case. Otherwise, it involves a combination of antituberculosis medications and supportive care. The standard treatment regimen consists of a four-drug variety: isoniazid, rifampin, pyrazinamide, and ethambutol. The initial phase of treatment typically lasts for two months, followed by a continuation phase of isoniazid and rifampin for an additional four to six months. The adjunct use of corticosteroid therapy is controversial and not routinely recommended. However, as used in the present case, it might reduce inflammation and the risk of pericardial constriction (not proven effective). Supportive care may include the use of nonsteroidal anti-inflammatory drugs (NSAIDs) if there are no contraindications to relieve pain and inflammation and diuretics to reduce fluid accumulation. In essence, early diagnosis and treatment are crucial in preventing complications such as cardiac tamponade, constrictive pericarditis, and heart failure. Close monitoring of the patient’s symptoms, medication adherence, and regular follow-up are vital for successfully managing this condition.
* Adenosine deaminase (ADA) is a protein cells produce throughout the body. It is associated with activating lymphocytes, which play a role in the immune response to infections. Conditions that trigger the immune system, such as an infection caused by Mycobacterium tuberculosis, may cause increased amounts of ADA produced in the areas where the bacteria are present. The ADA test is used along with other tests such as pleural or pericardial fluid analysis, AFB smear and culture, and PCR, i.e., the tuberculosis molecular testing, to help determine whether a person has a Mycobacterium tuberculosis infection of the lining of the lungs (pleurae) or pericardium.
**Rifater and Rifinah are two combined preparations of anti-TB drugs (available for use in the United States): Rifater is a combination of isoniazid, rifampin, and pyrazinamide used during the initial phase of treatment. Rifinah contains the active ingredients rifampicin and isoniazid. According to the CDC, several treatment regimens are recommended for TB disease, including the 4-month Rifapentine-moxifloxacin TB Treatment Regimen and the 6-month RIPE TB Treatment Regimen. The 4-month regimen is shorter, effective, and all-oral. It would be a preference for many patients and national TB programs, allowing faster cures and easing the burden on patients and the healthcare system. Healthcare providers can choose the appropriate TB treatment regimen based on drug-susceptibility results, coexisting medical conditions (e.g., HIV, diabetes), and potential for drug-drug interactions.
**Electrical alternans is defined as alternating QRS amplitude in any or all leads with no additional changes to the heart’s conduction system. This phenomenon is interpreted by the “swinging heart” from a significant amount of fluid surrounding the heart. However, electrical alternans can be seen in other circumstances, like supraventricular tachycardia and ventricular tachycardia, at a fast rate, among others.
Keywords:
tuberculosis, pericarditis, pericardial effusion
UpToDate:
Tuberculouss pericarditis
Constrictive pericarditis: Management and prognosis

An 88-year-old woman complained of a loss of appetite, generalized weakness for two weeks, and increasing SOB for five days. She had chronic heart failure
A 43-year-old woman, s/p mitral valve (MV) replacement (Bjork-Sheily) for mitral stenosis (MS) associated with rheumatic heart disease 18 years ago, was admitted with worsening
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.