Case 16
This 43-year-old woman was rushed to ER because of the sudden onset of substernal chest tightness accompanied by cold sweats, which lasted more than 30
A 20-year-old man awakened from sleep with severe chest tightness and shortness of breath (SOB). Simultaneously, he felt dizzy and nauseous and fainted with crutches while going to the bathroom. He had undergone internal nailing of a left femoral shaft fracture due to a motorcycle accident two weeks prior and had noticed progressive swelling of the left lower leg with pain for the past week. PMH was significant for mitral valve prolapse, for which he had been on propranolol 10mg BID. He had no fever, chills, orthopnea, or hemoptysis. At Emergency Department, he was noted to have a facial contusion with broken incisors. He was obese and apprehensive in respiratory distress but was mentally well-oriented. BP measured 112/70 mmHg, PR 130/min, and RR 30/ min. There was an audible G2/6 systolic murmur at LSB but no rales at both lung bases. Notably, the left calf was swollen with local heat, redness, and tenderness. Homan’s sign was strongly positive. Chest -X-ray was unremarkable, and ECG showed an S1Q3 with a tendency toward an incomplete right bundle branch block (RBBB) pattern. Laboratory data showed Hb 12.6 (N: 13-18) g/dL, Ht 38.8 (N: 40-54) %, WBC 11,000 /uL, ABG pH 7.437 (N 7.35-7.45), pO2 62 (N 75-100) mmHg, pCO2 31 (N 32-45) mmHg, HCO3 21 (N 20-26) mmol/L, BE -1.5 (N -2.0 – +2.0) mmol/L, SaO2 92.6 %, BUN 17, mg/dL, Cr 1.0 mg/dL, AST(GOT) 59 (N: 15-41) IU/L, CKMB 3.3 (N: <5.4) ng/mL, Troponin-I 0.94 (N: <0.5) ng/mL, PT 11.1 (C:11.0) sec, APTT 27.1 (C:30) sec, and normal electrolytes. D-dimer was 7730 (N: <500) ng/mL. Brain CT was negative; echocardiography showed RV enlargement with moderate tricuspid regurgitation, moderate pulmonary hypertension (45 mmHg estimated), and LV EF 61.5 %. Notably, echo-Doppler of peripheral vessels showed a thrombus in the left popliteal vein, and pulmonary CT unveiled filling defects in bilateral pulmonary arteries suggesting bilateral pulmonary embolism (PE). Accordingly, the patient immediately received enoxaparin and Warfarin anticoagulation therapy in the CCU.
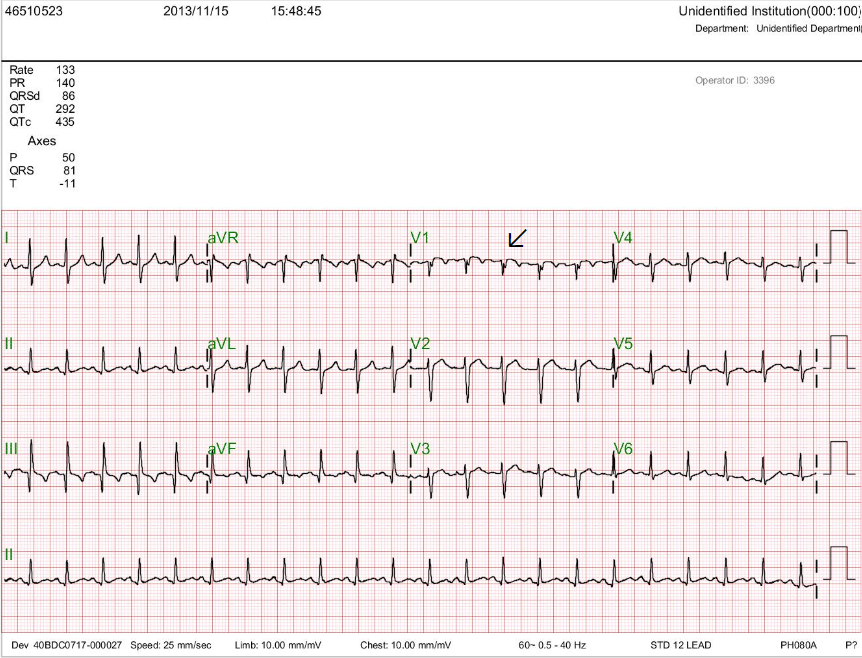
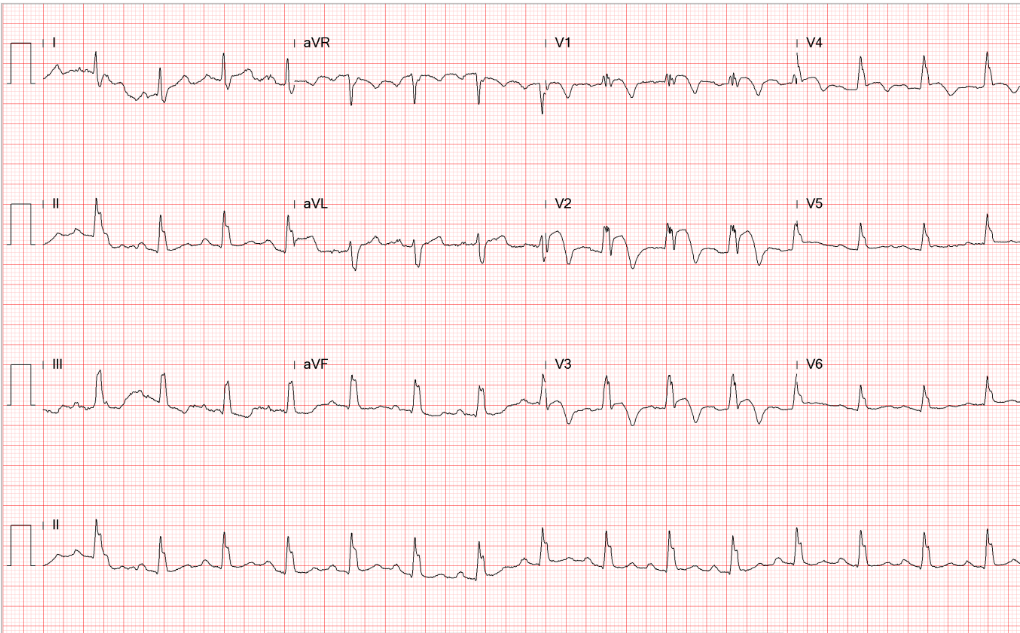
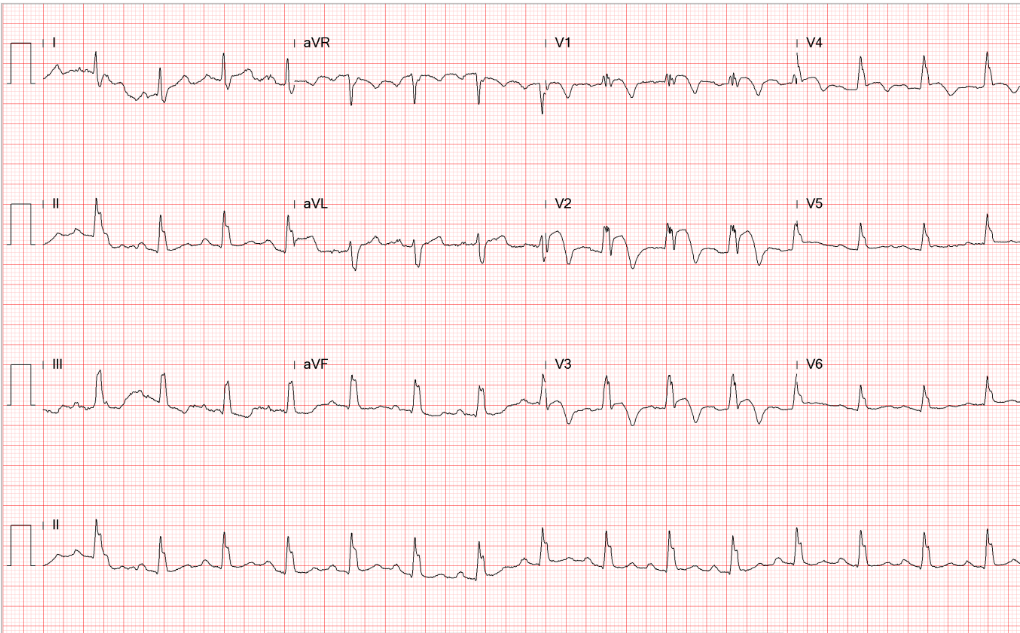
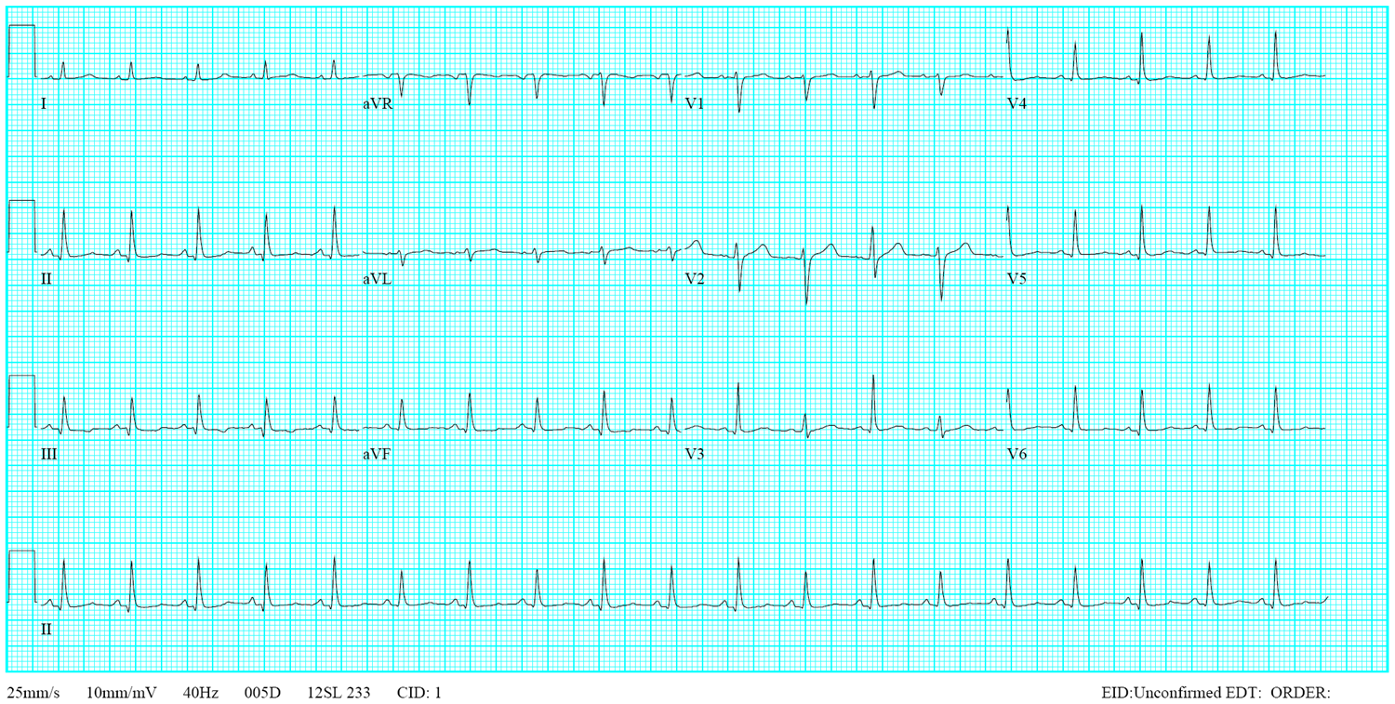
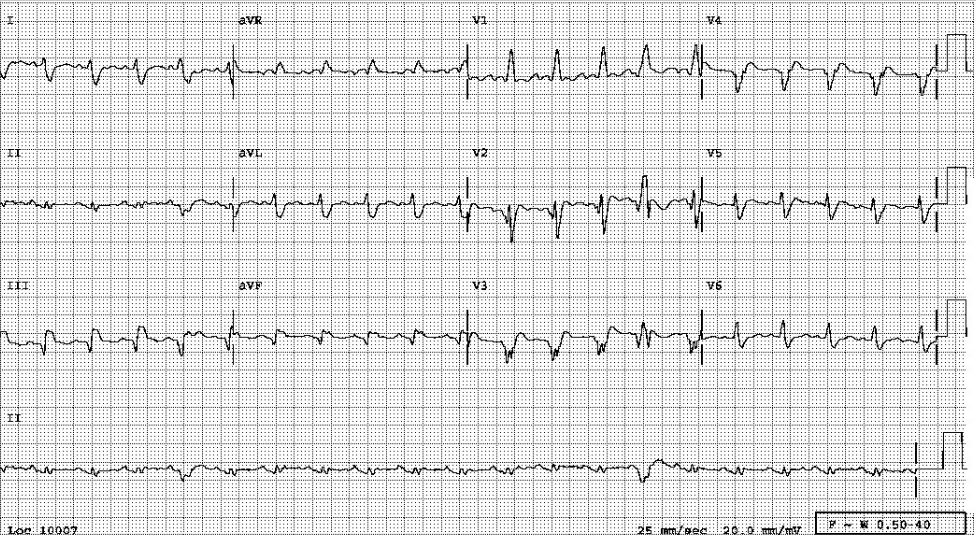
Sinus Tachycardia at 133/min.
Diffuse low QRS voltage.
QRS axis toward the right (+81 degree) with an S1Q3 pattern
Slow progression of the R wave in precordial leads (clockwise rotation of the heart).
Propensity to RBBB in V1 (a subtle finding indicated by an arrow).

Obesity with questionable cardiomegaly (AP view)
No definitive evidence of pleural effusion or heart failure
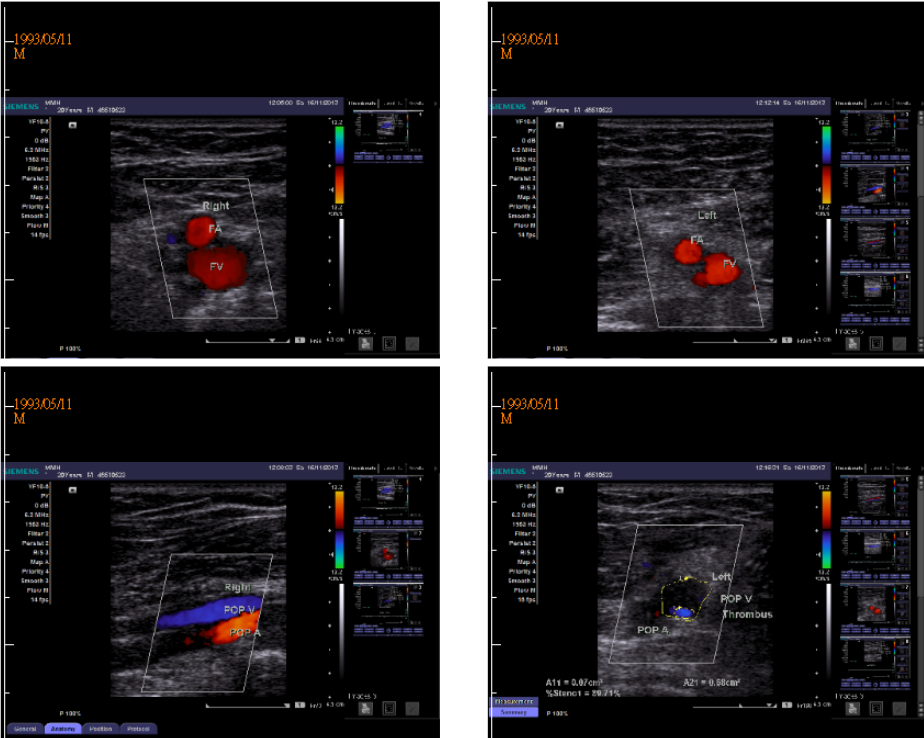
Thrombus in the left popliteal vein
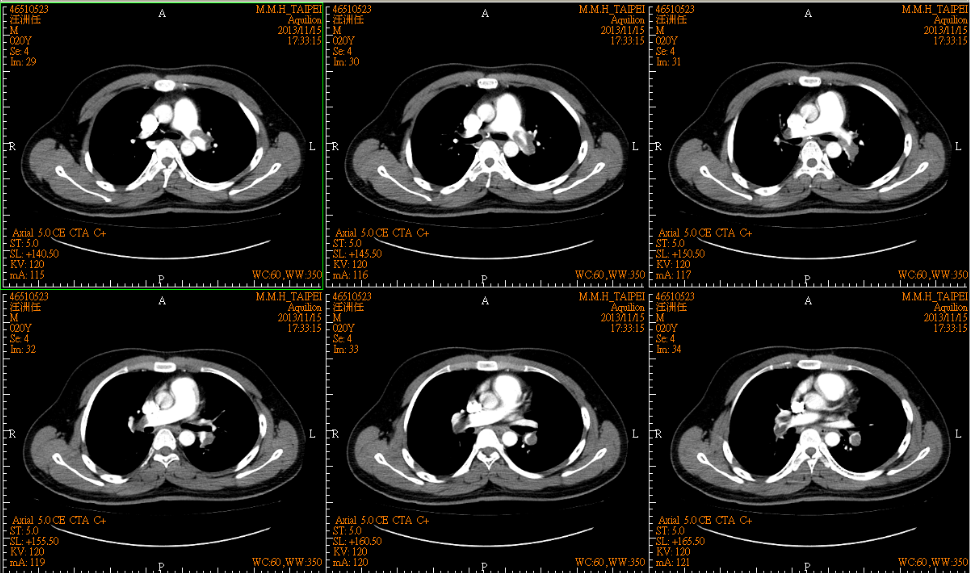
Intraluminal filling defects in bilateral PA consistent with bilateral pulmonary embolism.
RV enlargement with moderate tricuspid regurgitation.
Moderate PH with an estimated systolic pulmonary artery pressure is 45 mmHg.
LVEF 61.5 % with mild mitral regurgitation.
Sinus tachycardia is a typical feature in acute PE. The development of RV strain (ST depression or T wave inversion in V1-V3) (not seen in this case), S1Q3, or the right BBB pattern is in response to the sudden elevation in the RV pressure (N: <30/5 mmHg) resulting from PE. The presence of any of these latter findings suggests extensive PE. The increased systolic RV or pulmonary artery (PA) pressure (N: <30/10 mmHg) usually does not exceed 45 mm Hg in the first episode of acute PE; a reading higher than 50 mmHg indicates a preexisting chronic process, such as COPD with pulmonary hypertension (PH) or chronic thromboembolic PH, etc.
The ABG findings of hypoxia (pO2 62 mmHg) and hypoxemia (SaO2 92.6 %) alongside a relatively low pCO2 (31 mmHg) resonate with the initial stage of acute PE. Except for slight anemia, the elevation of the cardiac enzyme troponin-I (0.94 ng/mL) can be attributed to myocardial injury of RV resulting from a sudden increase in RV pressure due to acute PE.
While assessing a patient with suspected PE, it is crucial to identify signs and symptoms requiring resuscitative therapy (e.g., supplemental oxygen, hemodynamic or ventilatory support), such as severe chest pain or SOB, hemoptysis, hypotension, syncope, or near syncope. In the present case, the ECG findings and the history of immobility following internal nailing of a left femoral shaft fracture and thrombophlebitis of the left calf make the diagnosis of PE the highest probability. If such severe features are absent, physicians would usually proceed with revised Geneva (or Well’s) pretest probability scoring as described below:
Age 65 years or over (1)
Previous DVT or PE (3)
Surgery or fracture within one month(2)
Active malignant condition(2)
Unilateral limb pain(3)
Hemoptysis(2)
Heart rate 75 to 94 beats per minute (3)
Heart rate 95 or more beats per minute (5)
Pain on deep palpation (4)
The Geneva score so obtained relates to the probability of PE; 0 – 3 points indicate low probability (8%), 4 – 10 points intermediate probability (28%), and 11 points or more high probability (74%).
Patients with a high pretest probability, such as in the present case (Geneva score 14), should directly undergo CT pulmonary arteriograms (CTPA). Those with a moderate pretest probability should proceed with D-dimer testing first. If the D-dimer is normal, no further testing (except for a high clinical possibility) is necessary, and PE is excluded. If the D-dimer is elevated, then CTPA is required to rule out the diagnosis.
In patients younger than 50, the D-dimer is considered abnormal if it is greater than 500 ng/mL by an enzyme-linked immunosorbent assay [ELISA]. On the other hand, the D-dimer levels are considered abnormal above the patient’s age in years multiplied by 10 in patients older than 50 (e.g., 600 ng/mL for age 60, 700 ng/mL for age 70, etc.).
On the other hand, for patients with a low pretest probability for PE, further evaluation with the following questions (PERC criteria) are asked:
No further testing is necessary if all answers to the above questions are negative. However, if any of the questions listed above is positive, additional D-dimer testing is recommended, like the approach used for patients with a moderate pretest probability. Lastly, during the evaluation process, baseline laboratory studies should include renal function, a complete blood count, liver function, and baseline prothrombin/INR and partial thromboplastin times, as anticoagulation therapy might be necessary.
Keywords:
D-dimer, Geneva scoring, pulmonary angiograms, right ventricular strain
UpToDate:
Overview of acute pulmonary embolism in adults
Diagnosing and Treating Pulmonary Embolism in an outpatient setting or in Emergency Room:
This 43-year-old woman was rushed to ER because of the sudden onset of substernal chest tightness accompanied by cold sweats, which lasted more than 30
This 35-year-old male was transferred from a local hospital for further evaluation after a biopsy of a hard, 4 cm in diameter lymph node in
A 38-year-old man was admitted because of having abdominal fullness associated with progressive SOB (PND and orthopnea) for ten days. He denied having abdominal pain,
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung all right Reserved. Designed by 青澄設計 Greencle Design