Case 28
This 92-year-old man complained of progressive dyspnea with PND, productive cough with whitish sputum, and bilateral leg edema for the past few weeks. He was
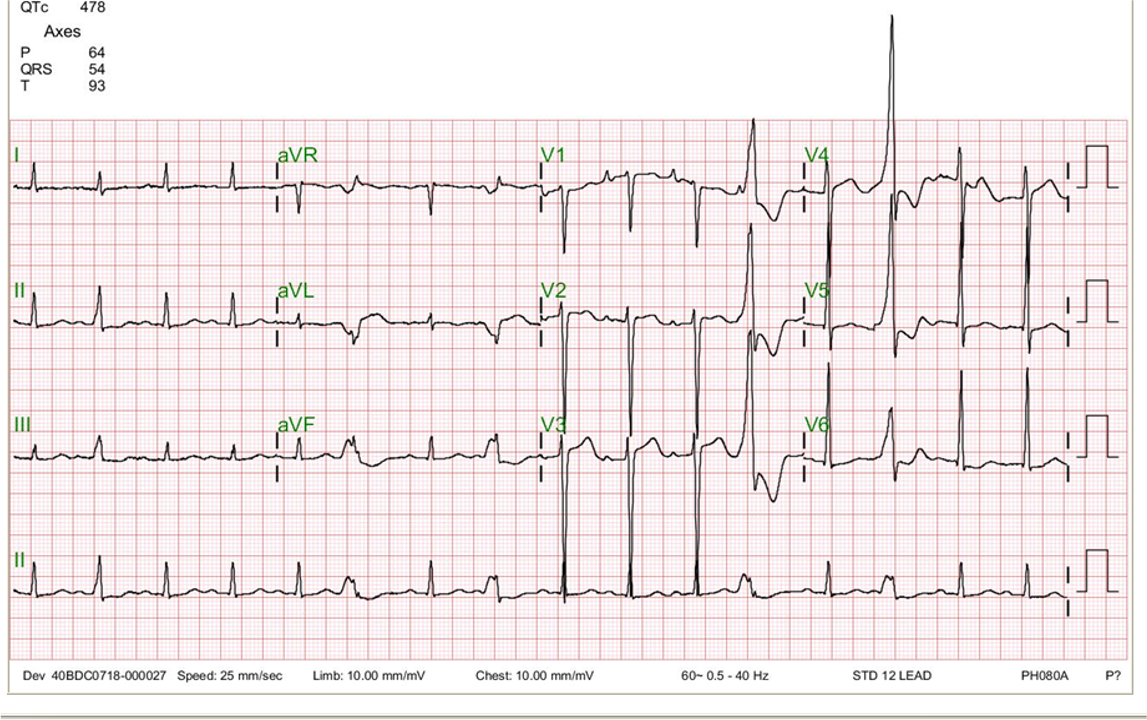
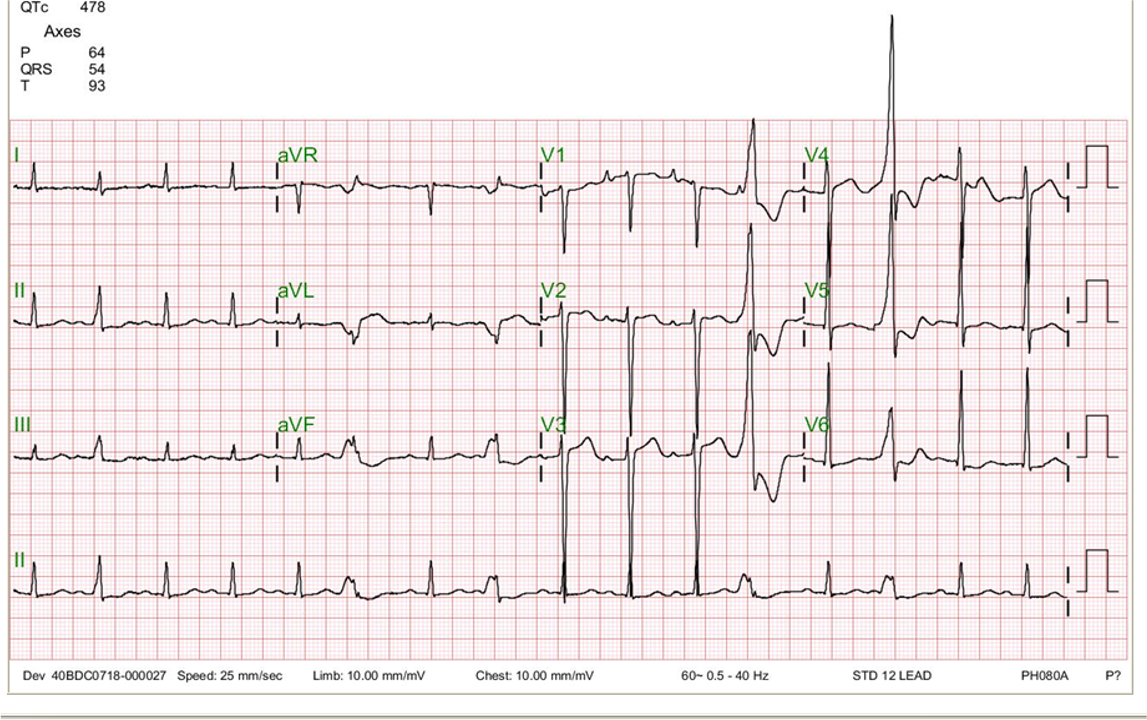
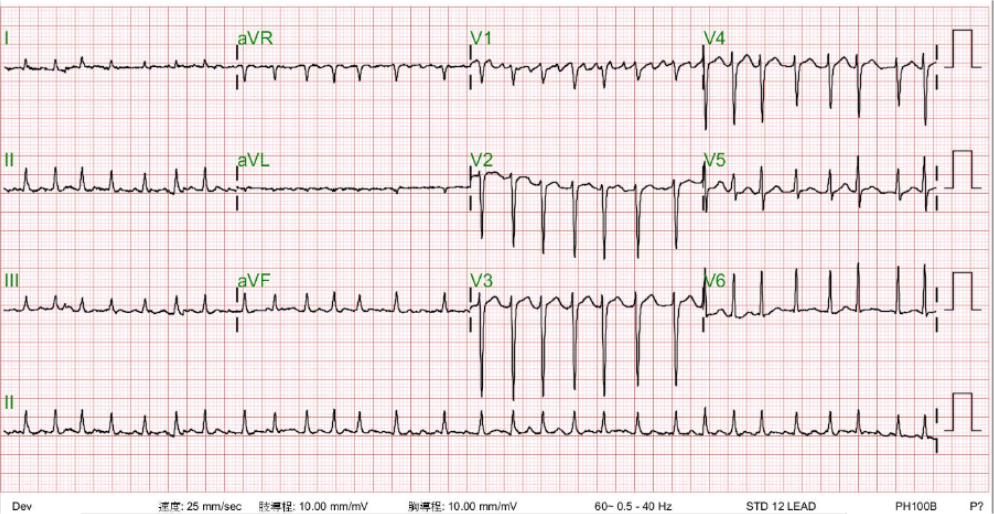
A 26-year-old Taiwanese man noted weakness in both lower legs and could not stand upon waking up. At the same time, he experienced upper back and arms pain and was brought to the Emergency Department (ED) in a wheelchair. There was no history of trauma, nor were there any signs of infection. PMH was significant in that he had hyperthyroidism (Free T4 47 [N 0.89-1.76] ug/dL, TSH <0.005 [N 0.40-4.0] uIU/mL), for which he was treated with methimazole for 28 days two years ago. Interestingly, his father also had hyperthyroidism diagnosed before. At Emergency Department, he appeared anxious and weak, in moderate respiratory distress, but was afebrile and mentally clear. BP measured 121/57 mmHg, PR 115/min, and RR 20/min. Physical findings were unremarkable except for a marked decrease in muscle tone and loss of deep tendon reflex (hyporeflexia) in both lower legs. ECG showed sinus tachycardia with diffuse nonspecific ST-T changes; The QT interval was within normal limits (QT 314 msec; QTc 382 msec). The chest X-ray illustrated no abnormality. Pertinent laboratory findings included Hb 16.2 gm%, Hct 47.6%, WBC 6.34K, Glucose 106 mg%, CPK 308 ng/mL, CRP 0.05, BUN 14.8 mg%, Cr 0.7 mg%, SGOT 36 [N 5-40] U/L, SGPT 55 [N 7-56] U/L*, Na 139 [136-146] mEq/L, K 2.1 [3.7-5.1] mEq/L, Cl 105 [96-106] mEq/L, Free T4 16.2 [N 0.7 to 1.9] ng/dL, TSH<0.01 [N 0.5 to 5.0] uIU/mL. The combination of hypokalemia and hyperthyroid state made the diagnosis of thyrotoxic hypokalemic periodic paralysis (THPP) a high priority.
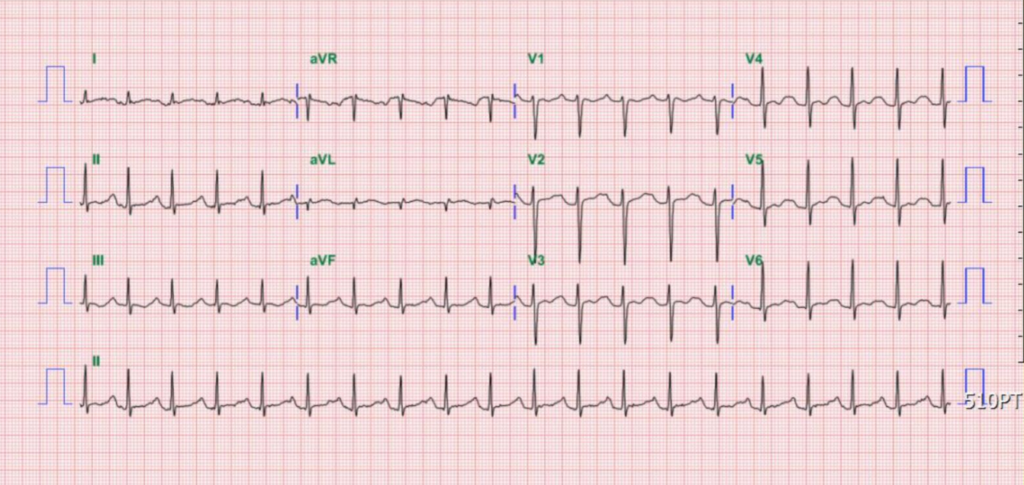
Sinus tachycardia at 115/min
Borderline PR interval at 200 msec
Diffuse nonspecific ST-T changes
QT 314 msec; QTc 382 msec
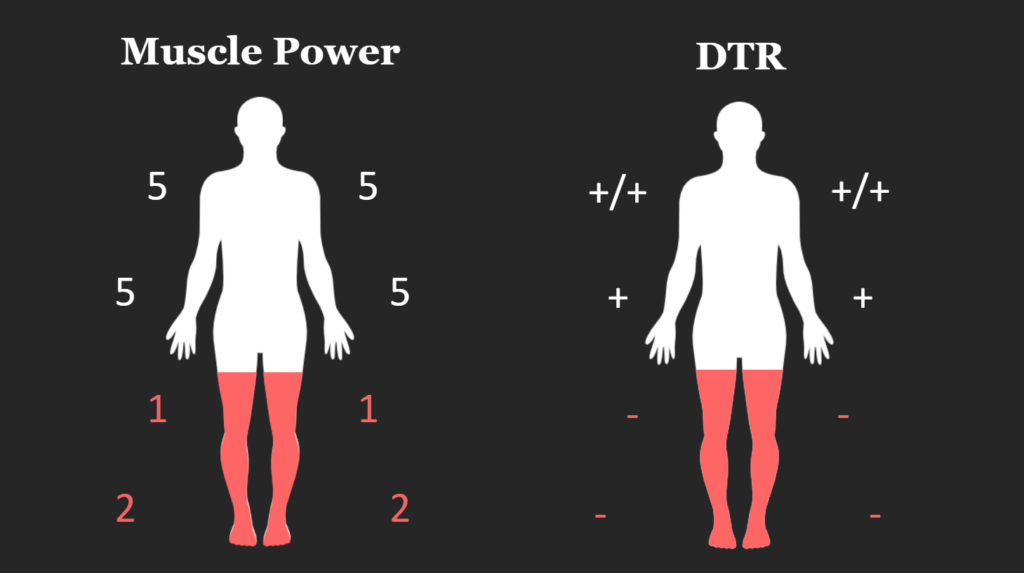
A marked decrease in muscle tone and loss of deep tendon reflex (hyporeflexia) in both lower legs
Although sinus tachycardia with nonspecific ST-T changes resonates with hyperthyroidism, it is too nonspecific to be diagnostic. The history, physical findings, and laboratory results (K 2.1 mEq/L, T4 16.2 ug/dL, TSH <0.01 uIU/mL) lean strongly toward the diagnosis of thyrotoxic hypokalemic periodic paralysis (THPP).
Contrary to hyperthyroidism in general, THPP is more prevalent in men (95%) than women, and there is a racial preference in East Asian men. The attack occurs more commonly at night, in the early morning, and in the summer. Exercise and a heavy meal (unclear in this case) might be the trigger. It is postulated that epinephrine and insulin directly or indirectly increase sodium-potassium ATPase activity on the skeletal muscle membrane. As a result, potassium is driven into cells, leading to hyperpolarization of the muscle membrane resulting in relative inexcitability of the muscle fibers. Excess thyroid hormone, on the other hand, increases the tissue responsiveness to beta-adrenergic receptors, thereby enhancing epinephrine and insulin-induced hypokalemic action.
Differential diagnosis includes a familiar form of periodic paralysis (genetically determined) or that related to an ion channelopathy (e.g., Andersen Tawil syndrome). It can be associated with hypokalemia, hyperkalemia, and normal serum potassium. Clinically, limb muscle weakness due to hypokalemia can also be seen in patients taking diuretics for hypertension or heart failure, mimicking THPP.
Additionally, in all patients with hypokalemia below 3.0 mEq/L, the development of lethal ventricular tachyarrhythmias such as ventricular tachycardia (VT) and ventricular fibrillation (VF) should be of utmost concern. Such patients should also have serum Mg and the QT interval measured and be carefully monitored while taking potassium supplements. Both hypokalemia and hypomagnesemia prolong the QT interval prone to torsade des pointes**, a specific form of malignant VT that can readily degenerate into VF, causing cardiac arrest. Lastly, besides correcting hyperthyroidism, a beta-adrenergic receptor-blocking agent (e.g., IV or oral propranolol) might also help improve leg weakness in patients with THPP.
*Liver enzyme elevation can be seen during hyperthyroidism.
** Torsades de Pointes (TdP) in French means a specific pattern of polymorphic VT on ECG that looks like twisting around a point or peak. TdP classically occurs in the setting of acquired or congenital long QT syndromes. It can lead to VF and thus causes cardiac arrest.
Keywords:
hyperthyroidism, QT interval prolongation, thyrotoxic hypokalemic periodic paralysis (THPP), torsades de Pointes (TdP)
UpToDate:
This 92-year-old man complained of progressive dyspnea with PND, productive cough with whitish sputum, and bilateral leg edema for the past few weeks. He was

A 62-year-old man was brought to Emergency Department for severe chest tightness of sudden onset, lasting 30 min. He had experienced episodes of chest tightness
An 81-year-old man came to the Emergency Department (ED) after one day of having progressive dyspnea with orthopnea and had diffuse itchy skin for more
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung all right Reserved. Designed by 青澄設計 Greencle Design