Case 2
A 58-year-old man, who had been in good health, became infuriated after a quarrel with his wife for 20 minutes. He suddenly experienced severe chest tightness with breathing difficulty and collapsed.
A 73-year-old woman, s/p ICD implanted for recurrent ventricular tachycardia (VT) associated with dilated cardiomyopathy (DCM) 9 months ago, was admitted after receiving several electrical shocks. These shocks caused arm pain and chest discomfort; the frequency was about once a week for five months. DCM was first diagnosed four years ago. Reportedly, coronary artery angiography was unremarkable then. She had no history of heavy alcohol drinking, but the family was positive for DCM (mother and one sister). She had been in NYHA functional class III, taking multiple medications, including carvedilol and amiodarone. These events of electrical shock usually occur while lying at night, without warning symptoms such as chest pain or palpitations. At admission, she appeared in moderate respiratory distress (BP 125/74 mmHg, PR 68/min, and RR 20/min). PMI was displaced 2cm to the left midclavicular line. There was a Gr 2/6 systolic murmur with an S3 at the apex, and there were bilateral crackles at the lower 1/3 of lung fields. Complete blood counts were normal, and so were serum electrolytes. The cardiac enzyme, Tn-I, was slightly elevated at 0.09 (N: <0.05 ng/dL). TSH and Free T4 levels were within normal limits (1.58 [0.5 to 5.0] mIU/L and 2.10 [0.7-1.9] ng/dL, respectively). BUN measured 22 mg/dL and Cr 1.38 mg/dL with an eGFR 40 mL/min/1.73 m2. ECG showed sinus rhythm at 68/min, intraventricular conduction defect (IVCD) or incomplete LBBB with LVH, and an old anteroseptal myocardial infarction (MI) pattern. Chest X-ray confirmed cardiomegaly and both RA and LA enlargement with pulmonary congestion. Echocardiography showed dilated LA and LV, global hypokinesis with LV EF 25 %, calcified MV annulus with severe MR, and mild pulmonary hypertension with mild TR. Interrogation of ICD documented actual episodes of VTs at 160-180/min triggering electrical shocks (not phantom)*. These ICD shocks were deemed appropriate, and VT episodes were provoked by worsening HF or vice versa at night. Accordingly, the therapeutic regimen was readjusted, and the treatment strategy was reassessed.
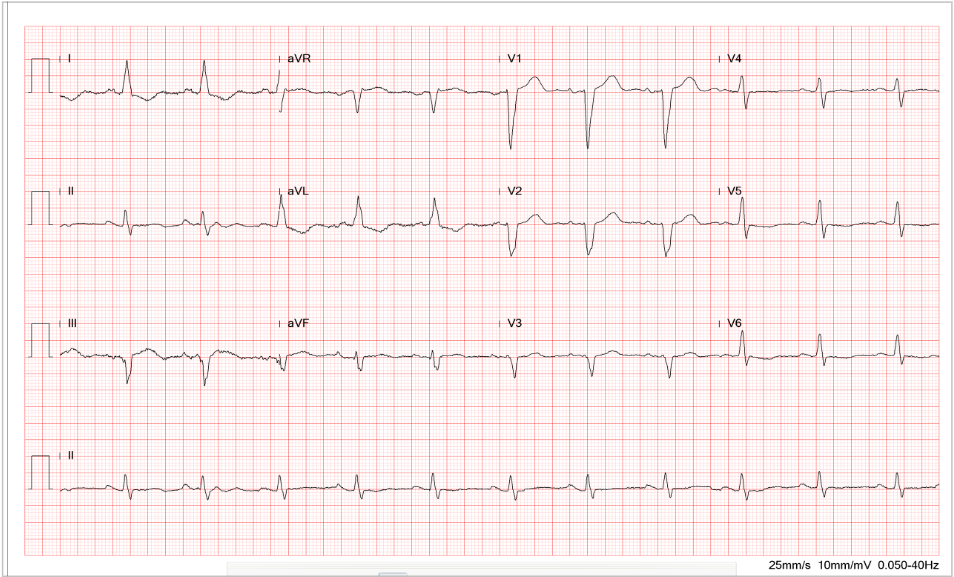
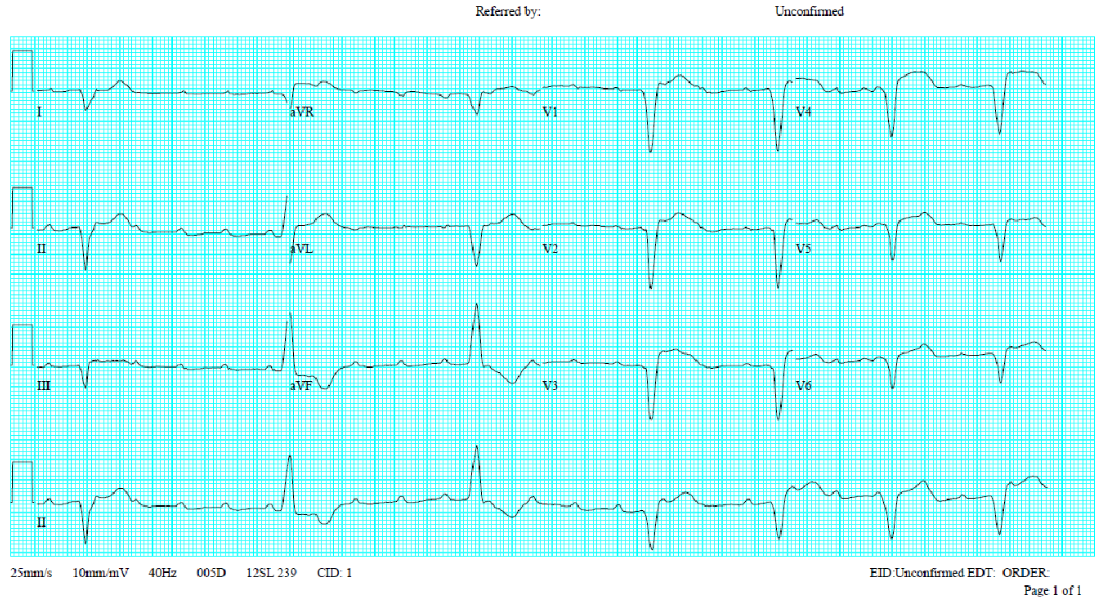
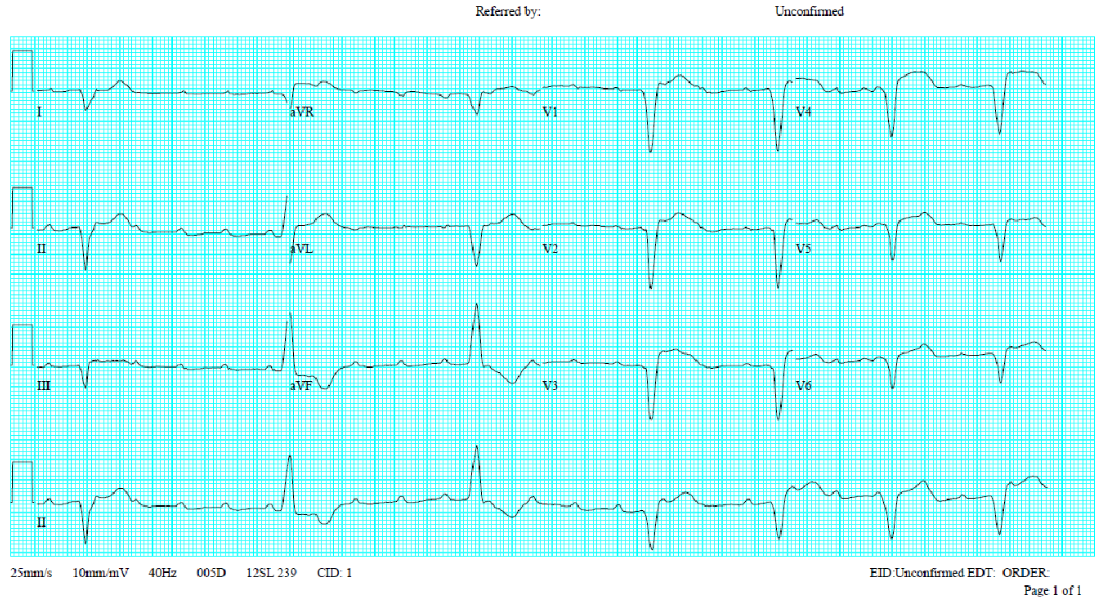
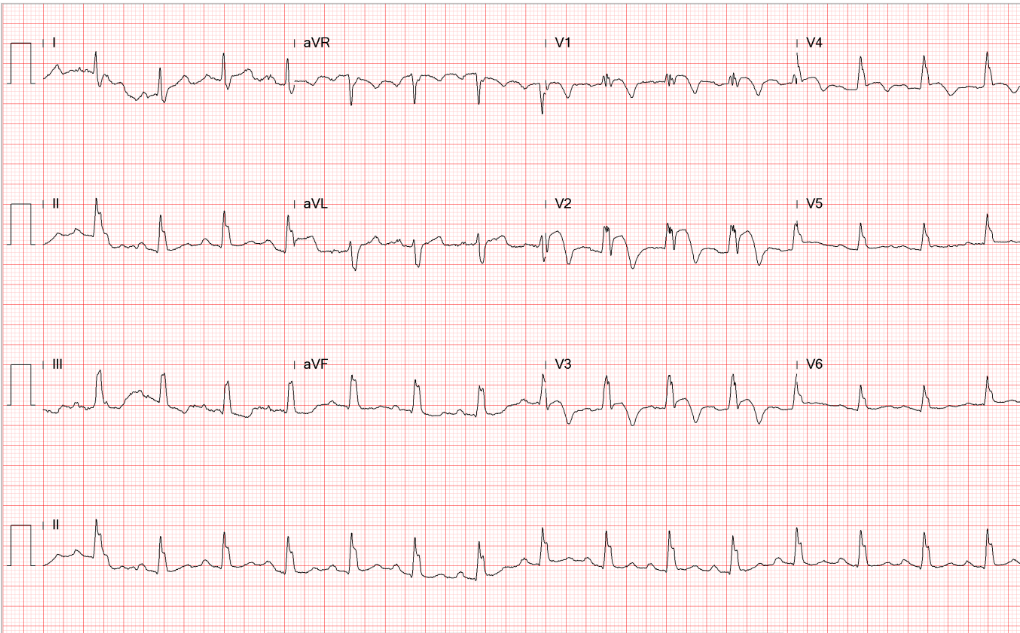
Sinus rhythm at 68/min
IVCD (QRSd 128 msec) or incomplete LBBB with LVH
Left axis deviation (-22°) probably due to left anterior hemiblock (LAHB)
Tiny r in V1-V3, r/o old anteroseptal MI
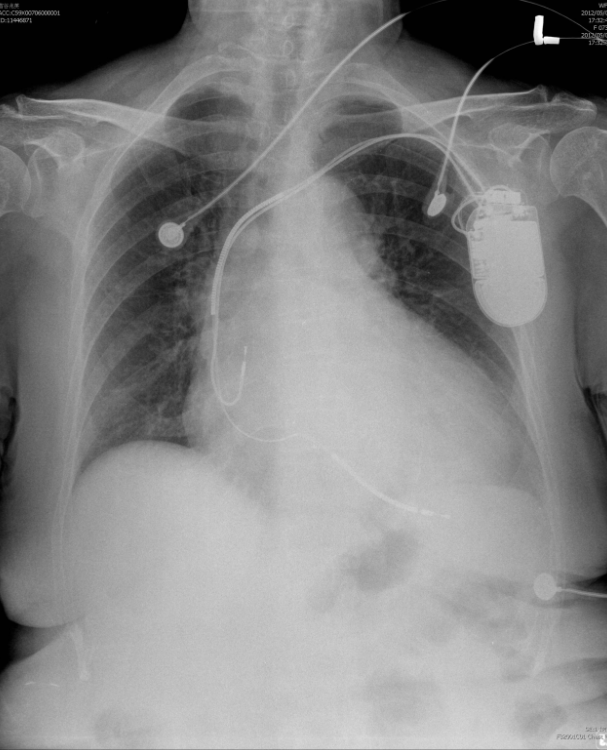
Cardiomegaly with LV, LA, and RA enlargement
Prominent PA with increased lung markings c/w pulmonary hypertension
Pulmonary congestion
A transvenous pectoral ICD pulse generator with its lead system in RA and RV
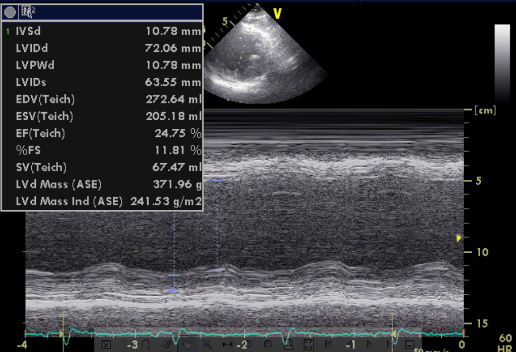
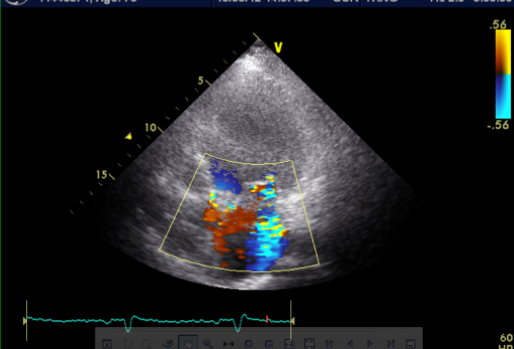
Dilated LA and LV, normal wall thickness global hypokinesis with LV EF: 25 %
Thickened and calcified aortic valve with mild AR.
Mitral annulus calcification with moderate to severe MR.
Mild TR with borderline PAH and mild pulmonary regurgitation
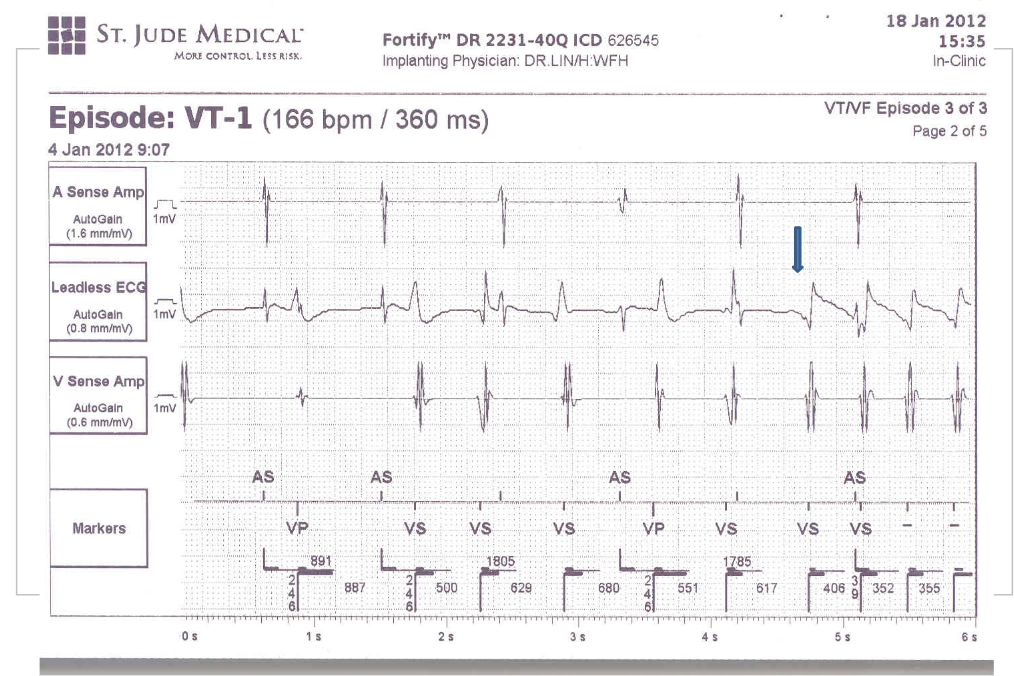
VT (blue arrow) emerges after the six V (VP+VS) signals.
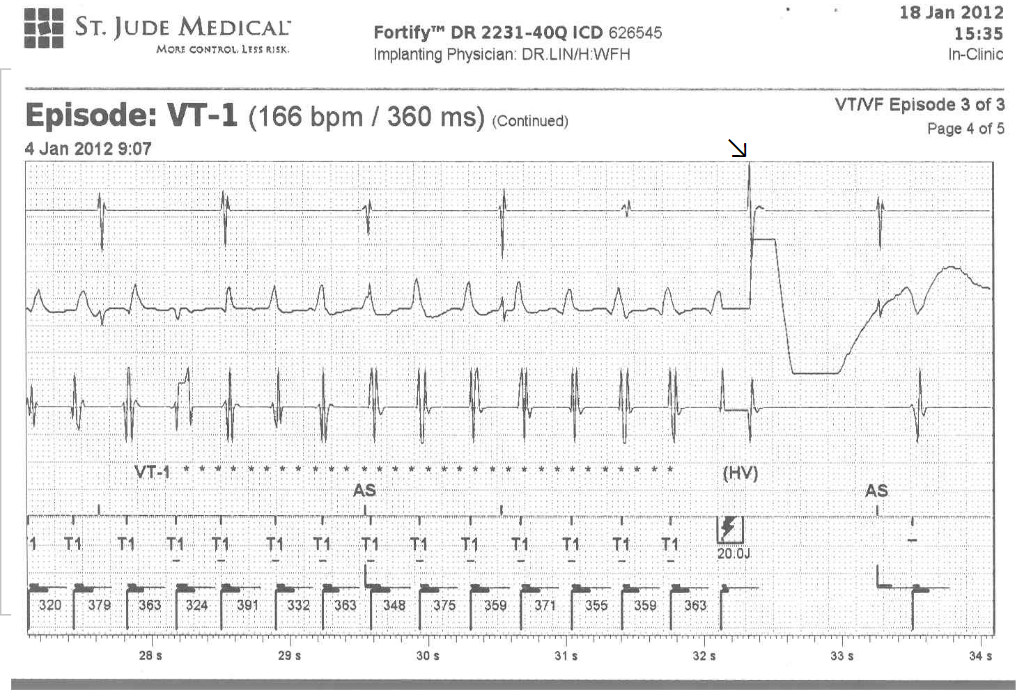
An ICD shock (red dot signal 20.0 J) terminates VT with an irregular cycle length of 320-391 msec.
The ECG patterns of MI and conduction disturbances (e.g., LBBB, LAHB) can be related to clinical conditions other than atherosclerotic coronary heart disease (CHD), such as in this case with DCM. They can also be seen with myocarditis, hyperkalemia, and other forms of cardiomyopathy (e.g., hypertrophic or restrictive). When LAHB-induced left axis shift is present, V6 registers an RS pattern, often masking the typical expression of LVH.
In general, sinus tachycardia usually resonates with HF. However, the sinus rhythm can be relatively slow, as seen in the present case (68/min), due to negative chronotropic properties of drugs (e.g., beta-blockers, amiodarone, etc.), sinus node dysfunction (i.e., sick sinus syndrome) or enhanced vagotonia.
Based on etiology, besides inherited (genetically determined) and idiopathic (no identifiable cause), DCM can be ischemic, stress-induced, infectious (e.g., viral, HIV, Chagas disease, Lyme disease), toxic (e.g., alcohol, cocaine, medications, trace elements, radiation), peripartum, arrhythmia (e.g., tachycardia, AF, PVCs, pacing-induced), sarcoidosis, end-stage kidney disease, endocrine dysfunction (e.g., hyperthyroidism, Cushing’s syndrome, pheochromocytoma), nutritional deficiency (e.g., thiamine, selenium, and carnitine), etc. Because of the family history, DCM is likely an inherited disorder in the present case.
Inappropriate ICD shocks can usually be ascribed to sensing of atrial tachyarrhythmias (e.g., AF or SVT) with a rapid ventricular response and, less often, electrical noise, inappropriate sensing, or ICD malfunction (e.g., insulation defect, artifact over-sensing, and lead fracture). On the other hand, appropriate ICD shocks triggered by the recurrence of VT/VF, as presented by the present case, the causes of which can be diverse. HF and tachyarrhythmias such as VT and AF are mutually causative. Under the circumstances, the differential diagnosis for the causative relationship between “HF triggering VT” and “VT worsening HF” is a clinical challenge.
Clinically it is not uncommon to see uncontrolled HF with “HF triggering VT.” The causes of uncontrolled HF include myocardial ischemia/infarction, electrolyte imbalance, adverse effects of drugs, uncontrolled hypertension, worsening HF, ineffective antiarrhythmic therapy (e.g., acute or chronic AF with a rapid ventricular response), etc. An individualized treatment strategy to correct the underlying etiology includes medical therapy for HF and VT, PCI (e.g., stenting), and surgery (e.g., CABG) for atherosclerotic CHD. Lastly, catheter ablation of recurrent VT or AF that triggers HF may be necessary. In many patients, better control of HF or avoidance of HF worsening is sufficient to prevent VT recurrence.
*Phantom shock — The patient’s perception of receiving an ICD shock when no shock is delivered.
Keywords:
dilated cardiomyopathy (DCM), implantable cardioverter/defibrillators (ICD), phantom shock, ventricular tachyarrhythmias (VT/VF)
UpToDate:
Causes of dilated cardiomyopathy
Cardiac implantable electronic devices: Long-term complications
A 58-year-old man, who had been in good health, became infuriated after a quarrel with his wife for 20 minutes. He suddenly experienced severe chest tightness with breathing difficulty and collapsed.
This 43-year-old woman was rushed to ER because of the sudden onset of substernal chest tightness accompanied by cold sweats, which lasted more than 30 minutes.

A 62-year-old man was brought to Emergency Department for severe chest tightness of sudden onset, lasting 30 min. He had experienced episodes of chest tightness unrelated to exertion for one year.
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung all right Reserved. Designed by 青澄設計 Greencle Design