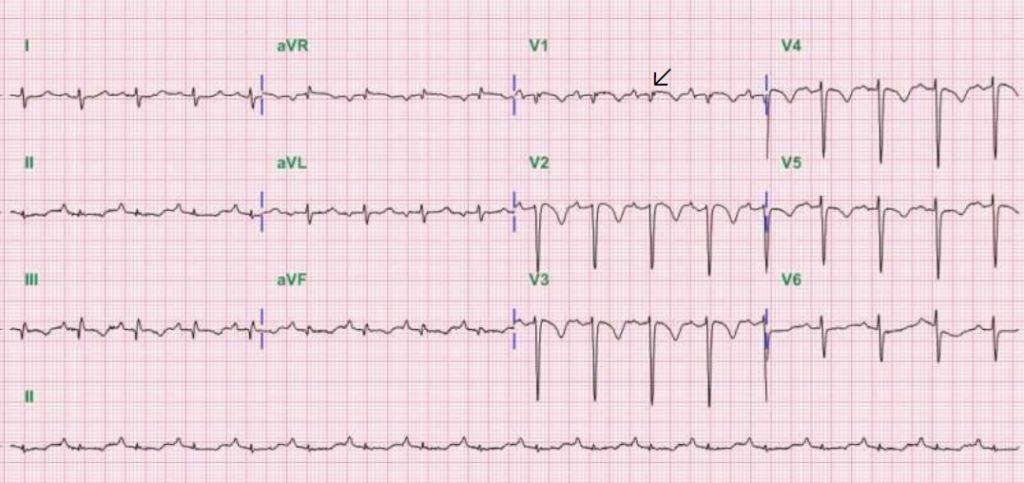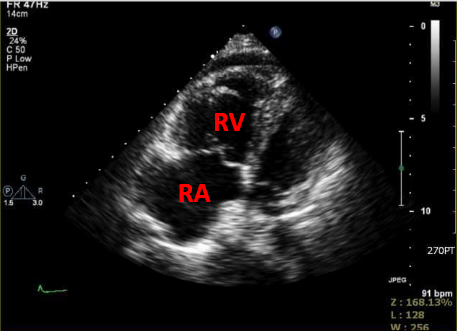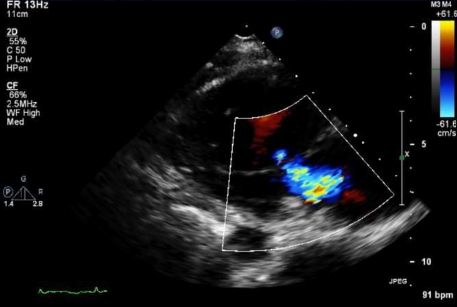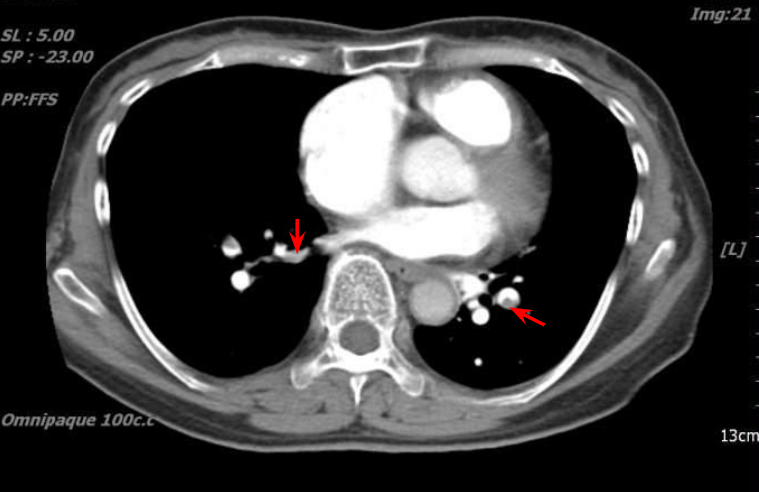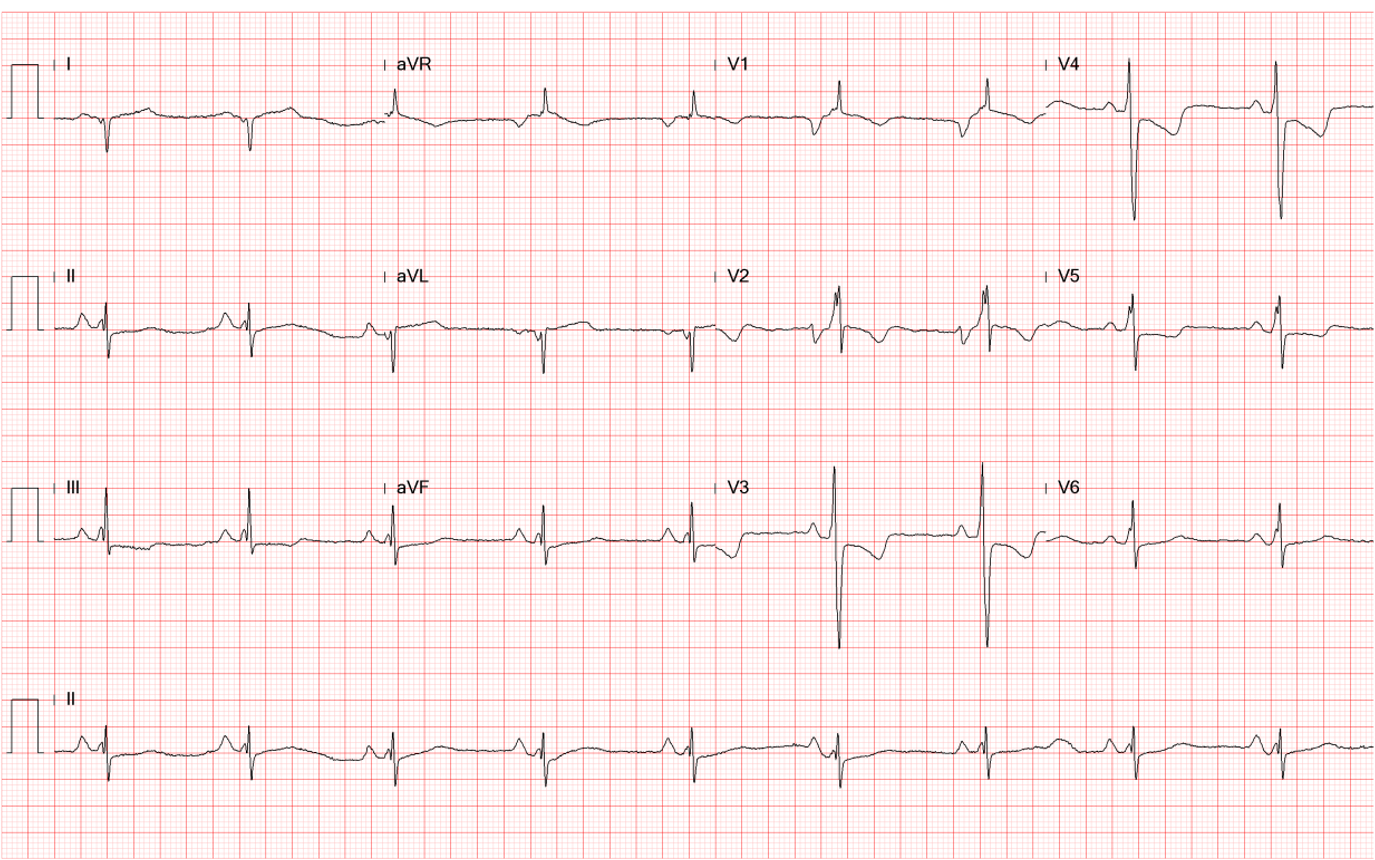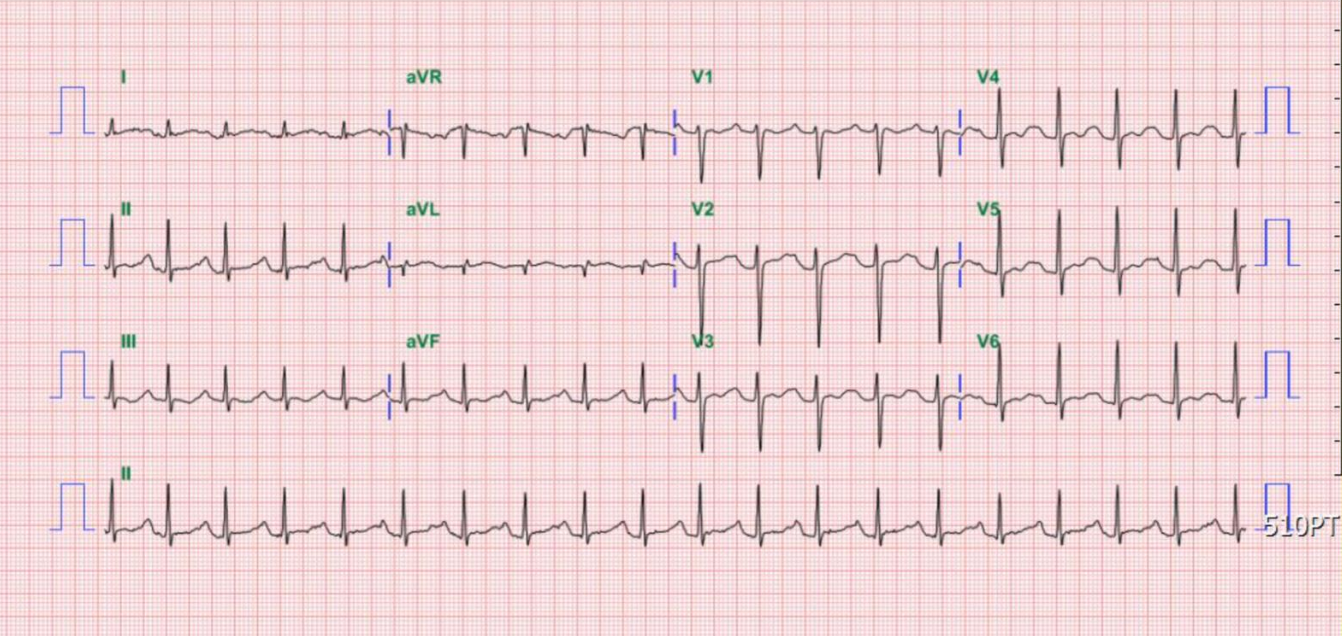
Case 4
A 26-year-old Taiwanese man noted weakness in both lower legs and could not stand upon waking up. At the same time, he experienced upper back and arms pain and was brought to the Emergency Department (ED) in a wheelchair. There was no history of trauma, nor were there any signs of infection.