回憶錄中文
生平簡介 宋瑞珍醫師是史丹佛大學和加州大學舊金山分校 (UCSF) 心血管醫學名譽教授。此前,他曾擔任史丹佛大學醫學中心「心臟電生理學和心律不整部」主任(1991-2001 年)。宋醫師畢業於國立台灣大學(1968 年),在威斯康辛大學完成住院醫師訓練(1970-72 年),並在邁阿密大學任職心臟病學研究員 (Fellow)(1972-74 年)。從那時起,他致力於臨床心臟電生理學研究。宋醫師率先
When this 78-year-old man walked into the clinic, he looked weary and depleted. For the past two days, he had been battling an intermittent fever topping 37.8°C, accompanied by a vanishing appetite and persistent exhaustion. He denied chills, symptoms of URI, dysuria, and diarrhea.
He had a long-standing history of hyperlipidemia, hypertension with chronic heart failure (HF), and chronic atrial fibrillation (AF) associated with non-obstructive hypertrophic cardiomyopathy. In addition, he had benign prostate hypertrophy with a previous UTI, thyroid nodules, a benign pancreatic cyst, low back pain due to lumbar spondylosis, and sleep apnea treated with Continuous Positive Airway Pressure (CPAP) but no diabetes or atherosclerotic coronary heart disease. Also of clinical significance, about one month prior, he had a VVI pacemaker prophylactically implanted for a ventricular pause of 3.6 sec recorded while asleep on Holter monitoring. Current medications include Atorvastatin 20 mg ¼ QD, Sacubitril/Valsartan 100 mg ½ QD, Amlodipine 5 mg QD, Trichlormethiazide 2 mg ¼ QD, Rivaroxaban 15 mg QD, Dutasteride 0.5 mg QD hs and Silodosin 4 mg QD hs.
He appeared slightly overweight, weak, and depressed but in no acute distress. BT/PR/RR measured 37.5 ºC, 70/min, and 15/min; blood pressure was 120/75 mmHg. There was no JVD, but there were crackles at the lung bases. The PMI was not visible, and a Gr 2/6 systolic murmur was heard at the apex. The rest of the physical findings were unremarkable. ECG showed AF with an average ventricular rate of 70/ min, and chest X-ray revealed cardiomegaly with a slight increase in pulmonary vascularity. Pertinent laboratory data included Hb 13.2 g/dL, WBC 6500/uL, CRP 2.3 (N <0.5) mg/L, BUN 12 mg/dL, Cr 0.9 mg/dL (eGFR 64.5 ml/min), GOT 11 (N <40) U/L, GPT 22 (N <40) U/L, Na 143 mEq/L, and K4.4 mEq/L.
The COVID-19 test was negative, and immediate urinalysis was not indicative. Moreover, the abdominal CT scan with a contrast medium showed no sign of infection. The care team also ruled out apathetic hyperthyroidism (TSH 3.573 (N0.550-4.770) mU/L, Free T4 1.20 (0.89-1.76) ng/dL) and collected blood and urine samples for cultures. As he elected to return home, the care team gave him one intravenous dose of 500 mg ceftriaxone (a third-generation cephalosporin antibiotic) and oral cefixime 200 mg b.i.d.
Three days later, while urine cultures showed no growth, blood cultures flagged positive for non-methicillin-resistant staphylococcus aureus. He was urgently admitted. Upon admission, he was in slight respiratory distress with delicate wheezing sounds. BT/PR/RR measured 38.2 ºC, 78/min, and 18/min; blood pressure was 110/70 mmHg. A repeated WBC was 12400 /uL and CRP 18.74 mg/L. The care team gave furosemide 40 mg for mild HF and ordered echocardiography. Transthoracic echocardiography showed non-obstructive cardiomyopathy with LA enlargement, moderate MR, preserved LV function (EF 55-60%), and no evidence of vegetations on the pacing lead and tricuspid valve. However, transesophageal (TE) echocardiography unveiled small vegetations on mitral and aortic valves (a 0.8 x 0.5 cm over mid-mitral P2 area and a tiny one over the aortic rim) indicative of infectious endocarditis.
Based on the sensitivity tests, the care team started intravenous oxacillin 2000 mg Q4H and gentamicin 80 mg Q8H. With staphylococcus aureus identified as the pathogen, the care team could not help but regard the recently implanted pacemaker as the infectious source and removed the pacemaker system on the third day of admission. Notably, removing the infected device unleashed intermittent fevers spiking up to 38.6°C and developing into a left-sided sore neck.
The gallium scan, followed by a CT scan with an intravenous contrast medium*, diagnosed and localized the sore spot as focal cellulitis with an abscess formation in the left-sided thyroid nodule, requiring aspiration (about 30 ml). The incidental thyroid function test showed T4 of 1.98 (N 0.92-1.68) ng/dL and TSH of 0.01 (N 0.27-4.20) mU/L. Accordingly, the care team added a low dose of methimazole 5 mg, qd, and switched oxacillin to dicloxacillin administered through a PICC (peripherally inserted central catheter). He then gradually became afebrile in four days. A week later, the relevant laboratory data showed Hb of 10.8 g/dL, Hct 30.7%, WBC 6580/uL, CRP 0.32 mg/L, BUN 32 mg/dL, Cr 1.6 mg/dL, (eGFR 45.6 ml/min), GOT 23 U/L, and GPT 25 U/L, along with TE echocardiography showing resolution of all vegetations.
During the four-week hospital stay, the care team noticed a significant decline in renal function with increased serum Cr from 0.9 to 1.6 mg/dL (eGFR decreased from 64.5 to 45.6 ml/min). They attributed it to gentamicin- and CT contrast medium-induced nephrotoxicity.** Throughout the course, whenever possible, an assistant helped him get up for a short walk, and he continued CPAP at night while asleep. A previous test had shown CPAP could significantly lower NT-ProBNP at night (930 decreased to 450 ng/L).*** After the completion of four weeks of intravenous antibiotic therapy, the care team discharged him with oral cephalexin 500 mg TID for two weeks. Lastly, while at home, he developed easy bruising with spontaneous subcutaneous hemorrhage. The latter finding alerted the care team of possible anticoagulant overdosage due to reduced renal function. Consequently, the care team decreased the dosage of rivaroxaban from 15 mg to 10 mg QD.****
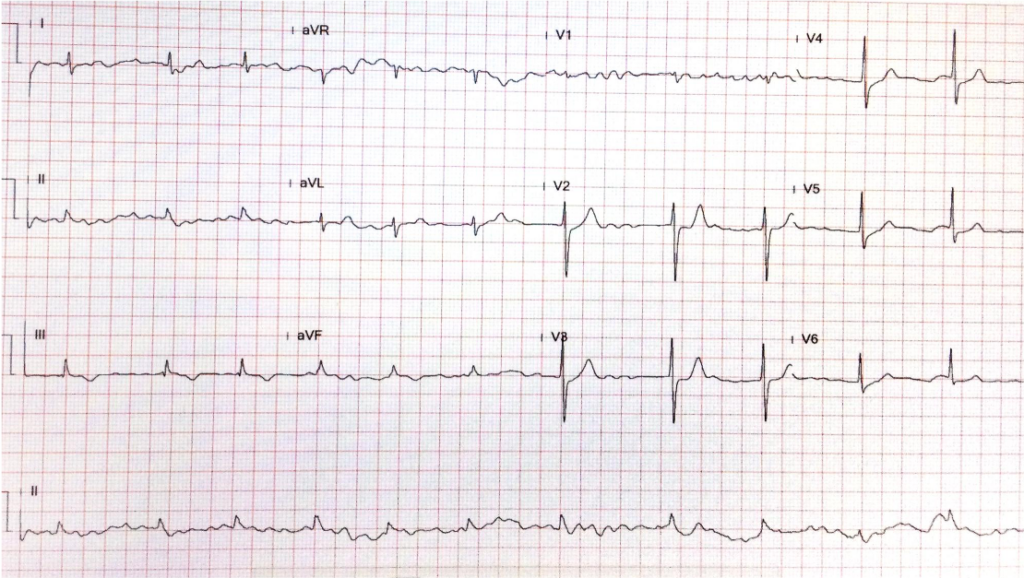
Diffuse low voltage likely due to body build
AF with an average ventricular rate of 70/min.
Nonspecific ST-T changes

Cardiomegaly (LVH) with LA enlargement (widened carina angle and double density)
Tortuous aorta with calcification on the knob
There is a slight increase in pulmonary vascularity
An implanted pacemaker with a single lead anchored in the RV apex
following removal of the pacemaker system.

The previous pacemaker system was removed.
Clinical interpretation
Despite having staphylococcus aureus endocarditis, characterized by positive blood cultures and valvular vegetations on echocardiography, the average ventricular rate of chronic atrial fibrillation in this patient measures only 70/min. During the initial clinic visit, the physician did not suspect a severe disease due to the absence of tachycardia and leukocytosis (6500 /uL). It appears that the patient’s response to infection, including sympathetic tone and immune reaction, is delayed due to their old age, which accounts for the “subacute” clinical presentation. There is also a possibility that associated atrioventricular nodal dysfunction, which is also related to old age, or adrenergic beta-receptor blocking agent therapy (not present in this case) may mask the tachycardia response in patients with severe infectious illness.
Pacemaker-induced bacterial endocarditis is an infection affecting the heart’s inner surface or valves. This infection can be caused by bacteria that enter the bloodstream during the implantation of a pacemaker or afterward. The presence of vegetation on the mitral and aortic valves (the left side of the heart) is a sign of hematogenous bacterial spread. Staphylococcus aureus is the most common pathogen found in these types of infections, but other bacteria like coagulase-negative staphylococci, streptococci, and enterococci can also cause the disease. The symptoms of the infection can occur suddenly (acute form) with high fever, chills, and systemic illness or have a more gradual onset (subacute form) with fatigue, weight loss, loss of appetite, and other nonspecific signs, especially in older patients.
Blood cultures and echocardiography confirm the diagnosis of this type of endocarditis. Managing pacemaker-induced infectious endocarditis involves antibiotic therapy and removing the infected hardware, including the pulse generator and pacing lead. However, removing the pacemaker system may cause further hematogenous spread of bacteria, as illustrated in the present case, so careful management is crucial.
The blood culture results typically guide antibiotic treatment and require consultation with an Infectious Diseases specialist. Prevention measures are also essential in clinical practice and include good hand hygiene, aseptic device handling, and prophylactic antibiotics before the procedure if necessary. Careful follow-up and monitoring for signs of infection in patients post-procedure. In high-risk patients, such as those with cancerous diseases, receiving immunosuppressive agents or previously infected implantable cardiac electronic devices, an absorbable antibacterial envelope and preprocedural intravenous antibiotics postprocedural oral antibiotics (e.g., pre-op: cefazolin 1 to 2 g IV; post-op: cefazolin 2 g IV TID for one day followed by ciprofloxacin 250 to 500 mg PO BID for seven days) are strongly recommended.
The development of hyperthyroidism during this case is intriguing. Although stress or an infectious process can provoke hyperthyroidism in the present case, clinicians should also consider other possibilities, such as excessive iodine consumption, which can lead to an overactive thyroid in susceptible individuals. This can occur through the Jod-Basedow phenomenon, a thyrotoxic state caused by iodine-containing compounds in patients with pre-existing autonomously functioning “thyroid nodules,” as this patient has.
While the bulk of the literature does not directly associate typical antibiotics with the induction of hyperthyroidism, a specific subset of antibiotics loaded with a significant amount of iodine, known as iodinated glycerol, can exacerbate thyroid function in susceptible individuals. Other well-known medications can provoke or exacerbate hyperthyroidism, such as amiodarone, interferons, lithium, and thyroxine.
Amiodarone is an iodine-rich drug used for arrhythmias that can cause both hypothyroidism and hyperthyroidism. Amiodarone-induced Thyrotoxicosis is associated with an excess iodine load that leads to increased synthesis of thyroid hormones in an abnormal thyroid gland (Jod-Basedow phenomenon). However, it can also cause destructive thyroiditis, leading to the release of preformed thyroid hormones from normal glands.
Interferons and other immunomodulatory drugs commonly used for treating multiple sclerosis and Hepatitis C may trigger autoimmunity, including Graves’ Disease. Lithium, while more commonly associated with hypothyroidism, can induce hyperthyroidism through its inhibiting effect on the release of thyroid hormones. This results in goiter formation with subsequent leakage of large amounts of thyroid hormone, causing “leak-induced” hyperthyroidism. It is noteworthy that these drugs do not induce hyperthyroidism in everyone, and they generally occur in individuals who already have an underlying thyroid condition, such as “thyroid nodules” or autoimmune susceptibility. Lastly, Over-replacement or misuse of levothyroxine can cause iatrogenic hyperthyroidism, which is not uncommonly seen in clinical practice.
*Gallium-67 citrate scintigraphy is a nuclear medicine imaging study based on the principle that gallium-67 (67Ga), a radiotracer, binds to transferrin and other proteins of iron metabolism. Once attached, inflammatory cells, particularly neutrophils and macrophages, take up these, which can be imaged. This technique can detect abscesses, osteomyelitis, lung infections, and certain malignancies. However, while gallium scans can be beneficial in detecting certain conditions, they do not provide the same anatomical detail as a CT scan. Therefore, they are often used with other imaging modalities for a more comprehensive evaluation. The test also has a relatively high radiation dose and a long acquisition time.
Intravenous contrast media used in computed tomography (CT) are typically iodine-based compounds. These contrast agents enhance the visualization of specific tissues or blood vessels during CT imaging. Currently used are non-ionic monomers or dimers. 1. Non-ionic monomers: These are low-osmolality contrast media (LOCM). They are now the most commonly used type of intravenous contrast in CT. 2. Non-ionic dimers: These are iso-osmolality contrast media (IOCM). They have the same osmolality as human blood, which can reduce the risk of adverse reactions. However, they are more expensive than LOCM. Most iodinated contrast media for CT scans contain 300-370 mg iodine/mL. The higher the iodine concentration, the greater the radiopacity and the better the enhancement of the tissues during imaging. The total amount of iodine administered to a patient during a CT scan depends on its concentration and the volume of the contrast medium dispensed. It’s important to note that the use of iodinated contrast media can carry risks, including allergic reactions and “contrast-induced nephropathy,” particularly in patients with pre-existing renal impairment. Therefore, the decision to use contrast and the choice of contrast agent should be made on an individual patient basis, considering the potential risks and benefits.
**Gentamicin-induced renal dysfunction (nephrotoxicity) is characterized by acute kidney injury (AKI), which can manifest as decreased urine output, elevated serum creatinine, and abnormal electrolyte levels. The diagnosis is primarily clinical, based on the temporal relationship between gentamicin administration and the onset of renal dysfunction. Laboratory tests play a crucial role in the diagnosis. These include monitoring serum creatinine (Cr) levels, blood urea nitrogen (BUN), and electrolyte levels. Urinalysis may show proteinuria and the presence of renal tubular epithelial cells.
In some cases, a renal biopsy may confirm the diagnosis, but this is usually reserved for cases where the diagnosis is unclear. The primary treatment for gentamicin-induced nephrotoxicity is the discontinuation of the drug. This often leads to improvement in renal function, although recovery may take weeks to months, and in some cases, the damage may be irreversible. Supportive care is also essential, which includes maintaining adequate hydration, correcting electrolyte imbalance, and avoiding other nephrotoxic agents (e.g., contrast media for imaging). In severe cases, renal replacement therapy (dialysis) may be required. The use of certain medications like N-acetylcysteine and sodium bicarbonate has been studied for the prevention and treatment of aminoglycoside-induced nephrotoxicity. Still, the evidence is not strong enough to recommend their routine use. Prevention is critical in managing gentamicin-induced nephrotoxicity:
It’s also important to closely monitor renal function in patients receiving gentamicin, especially those with risk factors for nephrotoxicity, such as advanced age, pre-existing renal disease, and concomitant use of other nephrotoxic drugs (e.g., gentamicin and CT contrast medium in the present case).
***CPAP has several effects on cardiopulmonary circulation. Firstly, CPAP improves oxygenation by increasing the functional residual capacity, reducing breathing work, and improving gas exchange, thereby benefiting obstructive sleep apnea, HF, and acute respiratory distress syndrome. Secondly, CPAP can reduce preload and afterload on the heart. By increasing intrathoracic pressure, CPAP decreases venous return to the heart, thereby reducing preload, favoring conditions like HF, where the heart is overloaded. On the other hand, by improving oxygenation and reducing hypoxic pulmonary vasoconstriction, CPAP can decrease pulmonary artery pressure and thus reduce the afterload on the right heart. Thirdly, CPAP can have a positive effect on LV function; CPAP can improve LV ejection fraction in patients with HF by reducing preload and afterload. However, it’s important to note that while CPAP can have beneficial effects on cardiopulmonary circulation, it can also have potential adverse effects. For instance, increased intrathoracic pressure can decrease venous return and cardiac output, particularly in hypovolemic patients. Therefore, careful patient selection and monitoring are necessary when using CPAP.
****Novel oral anticoagulants (NOACs) variably depend on renal clearance. Their dosages should be adjusted according to serum creatinine. Individual patient characteristics (e.g., age, body weight, etc.), comorbidities, and concomitant medications (i.e., drug interaction) should be considered when choosing and dosing a NOAC. Always refer to the specific prescribing information for each drug and consider consultation with a pharmacist or specialist in anticoagulation when managing these patients. Generally, with age ≥80 years, body weight ≤60 kg, or serum creatinine ≥1.5 mg/dL, the recommended dose for stroke prevention in AF should be reduced to half of the standard dosage. Rivaroxaban is eliminated by metabolic degradation through the liver (approximately two-thirds) and by direct renal excretion of unchanged compound (about one-third of the administered dose). Therefore, it was reasonable for the care team to reduce the dosage of rivaroxaban from 15 mg to 10 mg per day in the present case.
Keywords: complications of pacemaker implantation, drug-induced kidney
Injury, infective endocarditis, Jod-Basedow phenomenon
UpToDate: Overview of management of infective endocarditis in adults
Clinical manifestations and evaluation of adults with suspected left–
sided native valve endocarditis
Complications and outcome of infective endocarditis
1.Staphylococcus aureus endocarditis may present as a subacute onset.
Yes ( ) or No ( )
2.Removal of the pacemaker system is always necessary in pacemaker-induced
bacterial endocarditis.
Yes ( ) or No ( )
3.Contrast media used for CT scans may induce hyperthyroidism due to its iodine content.
Yes ( ) or No ( )
4.CRP is less sensitive than WBC in reflecting inflammation.
Yes ( ) or No ( )
5.Antibiotic therapy for bacterial endocarditis is 4-6 weeks.
Yes ( ) or No ( )
Answers: Y Y Y N Y
生平簡介 宋瑞珍醫師是史丹佛大學和加州大學舊金山分校 (UCSF) 心血管醫學名譽教授。此前,他曾擔任史丹佛大學醫學中心「心臟電生理學和心律不整部」主任(1991-2001 年)。宋醫師畢業於國立台灣大學(1968 年),在威斯康辛大學完成住院醫師訓練(1970-72 年),並在邁阿密大學任職心臟病學研究員 (Fellow)(1972-74 年)。從那時起,他致力於臨床心臟電生理學研究。宋醫師率先
This 30-year-old woman complained of having had about ten episodes of syncope associated with mild exertion for the past six months.
A 57-year-old woman with a long-standing history of bronchial asthma and COPD was admitted because of intermittent episodes of dyspnea associated with palpitations and general weakness for five days.
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.