
Case 9
A 67-year-old woman experienced progressive dyspnea with PND and leg edema for two weeks. PMH was significant for chronic hypertension for 20 years.
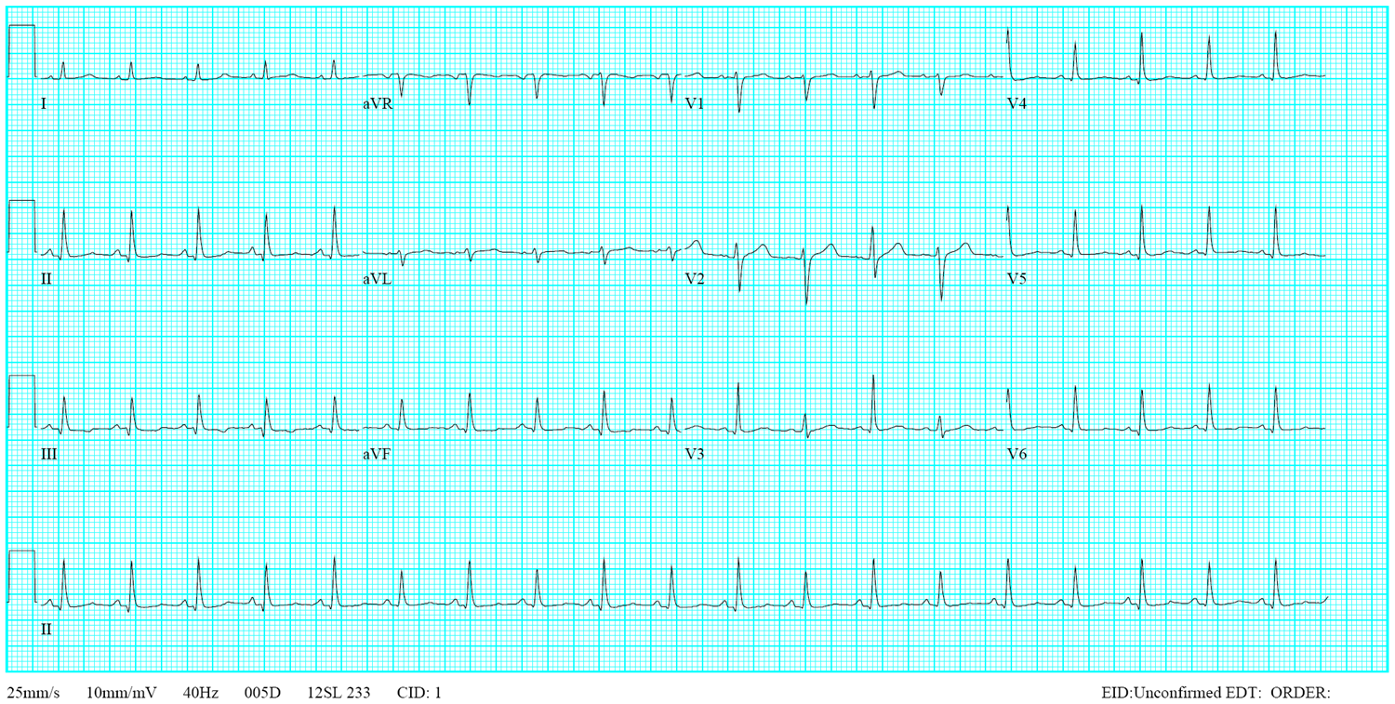
This 72-year-old man, a retired coal miner with a known history of chronic obstructive pulmonary disease (COPD) and pneumoconiosis, came to the Emergency Department complaining of increasing SOB for two days. He also had prostate hypertrophy with dysuria for several years. Past medical history is significant for atherosclerotic coronary heart disease (CHD), hypertension, s/p successful cavotricuspid isthmus ablation for atrial flutter, s/p pigtail insertion for a left-sided pneumothorax six months prior, and s/p MRI-conditioned DDDR permanent pacemaker implantation* for sick sinus syndrome five months earlier. On arrival, he appeared chronically ill and malnourished but mentally clear. He was in respiratory distress with effort breathing, BT/PR/RR measured 37 °C, 100/min, and 20/ min, respectively, and blood pressure was 130/80 mmHg. The pulse oximeter showed O2 desaturation (SpO2) of 80 (N 95-100) %**. There was a noted increase in the P-A diameter of the chest, and bilateral wheezes and basilar rales were audible. Heart sounds were distant. The rest of the physical findings were unremarkable. ECG showed diffuse low voltage, sinus tachycardia at 110/min and a relatively prominent P wave. Chest X-ray revealed hyperinflated lungs, bilateral interstitial nodules, and fibrotic or infiltrative changes. Additionally, there was bilateral blunting of the costophrenic angles suggestive of pleural effusion. The peripheral venous gas blood analysis (PVBG) study showed a pH of 7.403. Other laboratory data included Hb 11.2 g/dl, Hct 34.0%, Plt8, WBC 6770/ul, Na 139, K 4.7 , BUN 20 mg/dl, and Cr 0.88 mg/dl. Notably, urinalysis showed >30 WBC/HPF with a positive leukocyte esterase test, suggesting pyuria; later, urine culture grew out of Escherichia coli (colony count >100,000/mL ESB [extended-spectrum β-lactamase isolates])***. Although the patient was afebrile and there was no leukocytosis, the care team suspected possible pneumonia and urinary tract infection r/o septicemia as the cause of acute exacerbation of his breathing difficulty. Based on the urine culture sensitivity test, the care team started antibiotic therapy with doripenem in addition to bronchodilators. The patient then developed a productive cough with yellowish sputum and more breathing difficulty due to sputum impaction but remained afebrile and had no leukocytosis. The care team further added steroid therapy (methylprednisolone) and anticholinergics. Subsequent sputum culture was positive for Acinetobacter baumannii. According to the sputum culture sensitivity test, the care team added ceftazidime oligomycin inhalation and switched doripenam to gentamycin. An intravenous pyelography was performed on the 5th hospital day, and it revealed bilateral hydronephrosis and a dilated bowel (paralytic ileus). On the sixth day, he suddenly developed dizziness and vertigo. BT/PR/RR were 37 C/140/min, irregular/20/min, BP measured 95/61 mmHg, SpO2 97% under nasal O2 1-4 L/min. The corresponding ECG (ECG 2) showed AF with a rapid ventricular rate of 164/min, the chest X-ray revealed progressive infiltrates at bilateral lung fields, and ABG showed pH 7.448, pO2 88.8 mmHg, pCO2 48.4 mmHg, HCO3– 31.2 BE O2Sat 97%, Hb 12.7, Hct 39.2 WBC 21,590/ul with a left shift (Neutrophil [seg] 93%, [band 2] 2%)****, CRP 4.7 (N <0.5) mg/dl. The care team tapered bronchodilators to control AF and started intravenous amiodarone, oral propafenone, and verapamil. Cardiac enzymes remained within normal limits. Despite antiarrhythmic therapy, atypical atrial flutter***** with 2:1 conduction with a ventricular rate of 175/min emerged. Since then, his clinical course spiraled downward, and he succumbed to death on the 8th day.
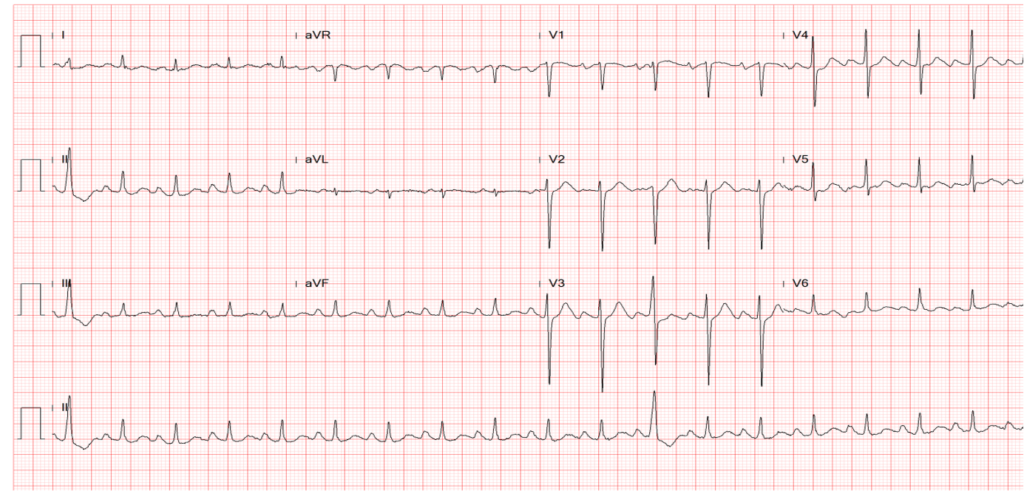
Diffuse low voltage
Sinus tachycardia at 110/min with a relatively prominent P wave ECG 2
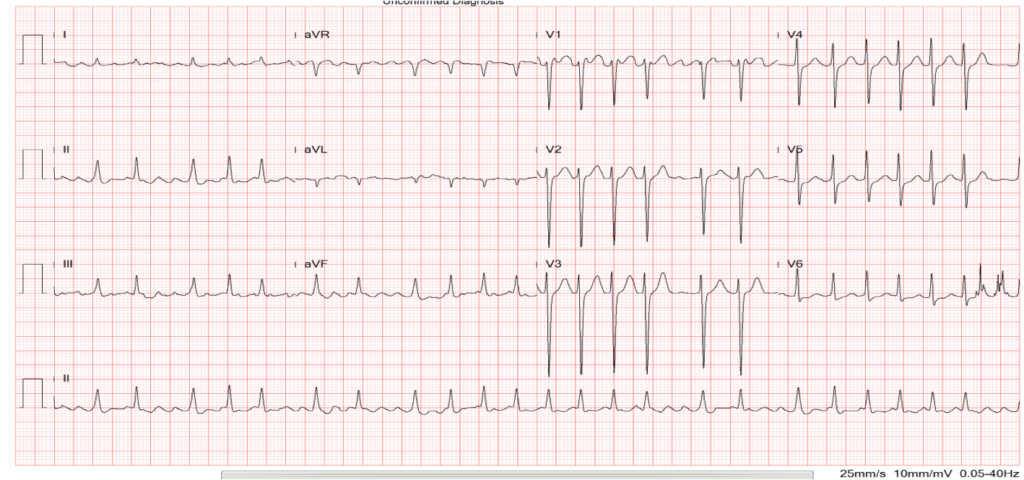
Diffuse low voltage
Atrial fibrillation with a ventricular rate of 164/min
Clockwise rotation of the heart
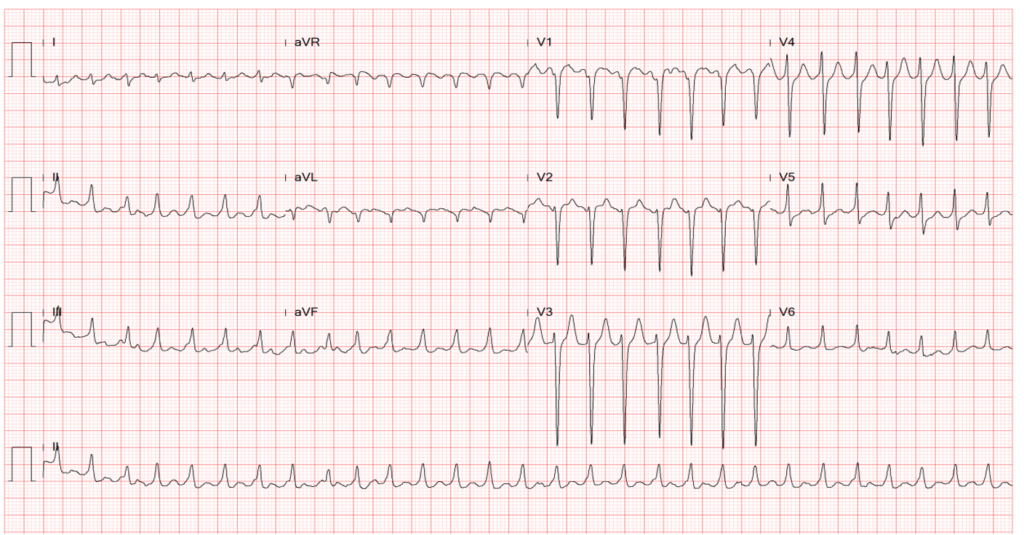
Diffuse low voltage
Atypical atrial flutter with 2:1 block – ventricular rate of 175/min
Clockwise rotation of the heart

Hyperinflated lungs,
Bilateral interstitial nodules and fibrotic or infiltrative changes
Bilateral blunting of the costophrenic angles (R>L) suggestive of pleural effusion
A dual-chamber pacemaker in place
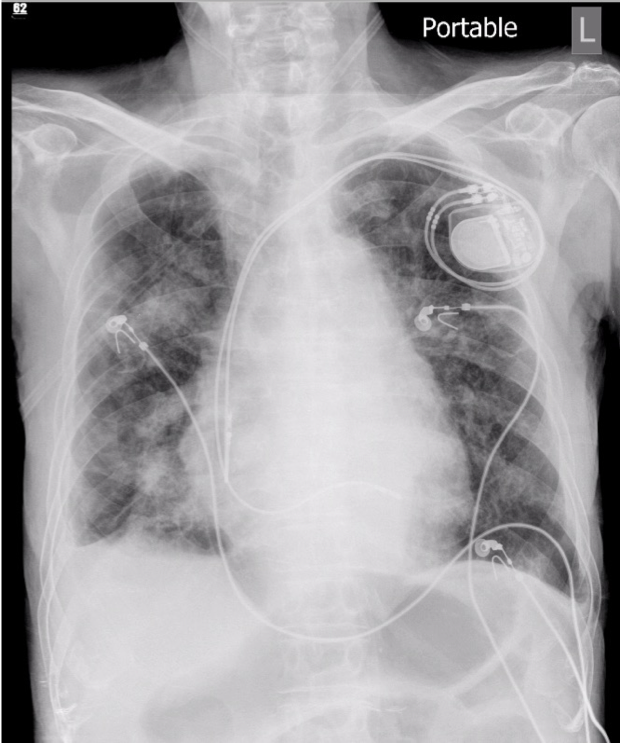
Progressive infiltrates at bilateral lung fields compared with the previous study
A dual-chamber pacemaker in place
The ECG findings of diffuse low voltage and clockwise rotation (more visible in ECGs 2 and 3) resonate with COPD. Sinus tachycardia is likely a response to hypoxemia.** Pneumoconiosis itself is not known to produce any specific ECG features. It is a chronic lung disease caused by inhaling certain dust particles that damage the lungs. It can be fibrogenic (e.g., silica, coal, talc, asbestos), benign or inert (e.g., iron, tin, barium), granulomatous (e.g., beryllium), and giant cell pneumonia (e.g., cobalt). The condition usually takes years to develop. Simple pneumoconiosis causes a small amount of scar tissue in the lung. Complicated pneumoconiosis can show progressive massive fibrosis (PMF).
The chest x-ray findings for pneumoconiosis are generally non-specific. Some expected results may appear in certain situations, like pleural plaques in asbestosis (a pathognomic sign) and interstitial nodules in the lungs, usually seen in silicosis and coal miners, as shown in the present case. PMF can also be seen in both silicosis and coal workers. In the present case, the chest X-ray findings also contain areas of hyperinflation, pleural effusion, and possible pneumonic infiltrates. Simple pneumoconiosis may have no or few symptoms, but PMF may cause mild to extreme difficulty breathing, like in the present case.
Currently, there is no cure for COPD and pneumoconiosis, so treatment aims to control symptoms and prevent the disease from worsening. From a functional standpoint, pneumoconiosis is a restrictive lung disease, whereas COPD (pulmonary emphysema or bronchial asthma) is an obstructive lung disease. Nonetheless, either can reduce pulmonary function capacity, impairing the exchange of O2 and CO2 and causing hypoxemia (pO2 <60 mm Hg), leading to tissue hypoxia.** Prolonged hypoxia can cause organ system damage. The organs most affected by hypoxia are the brain, the heart, the liver, and the immune system. If the hypoxia is severe, irreversible damage can begin within four minutes of the onset, and patients may develop headaches, dizziness, coma, seizures, and even death.
Patients with chronic lung disease often have comorbidities, in particular, cardiovascular diseases. Under the circumstances, the use of multiple drugs may cause drug interaction. Besides, certain medications (i.g., beta-agonists, anticholinergics, etc.) that are beneficial for the lungs might harm the heart, and vice versa. The emergence of AF and atypical atrial flutter***** is likely triggered by enhanced sympathetic tone in response to hypotension and hypoxemia related to worsening of infection, but also drugs like beta-agonists and anticholinergics. Anticholinergics reduce gastrointestinal motility by blocking muscarinic cholinergic receptors, which can result in constipation and, in severe cases, paralytic ileus, as in the present case. Furthermore, administering numerous antibiotics can further complicate the situation as these antibiotics are potentially harmful to many organ systems like the liver and kidneys.
The response in body temperature and leukocytosis to bacterial infection is often delayed in elderly patients, as illustrated in the present case. The sudden jump of the WBC count from 6,770 to 21,590/ul with a left shift (appearance of 2% band neutrophils) is intriguing. It reflects the worsening of infection as suggested by a progression of pulmonary infiltrates (Chest X-rays). However, to some extent, it can be attributed to “steroid-induced leukocytosis.”**** Given his age and the severity of pulmonary diseases with multiple comorbidities and complications in the past, the prognosis can be deemed grim on admission. Furthermore, both strains of bacteria, Escherichia coli in the urine and Acinetobacter baumannii in the sputum, are gram-negative bacteria, prone to be antibiotic resistant***, and difficult to eradicate, especially in debilitated elderly like the present patient.
* An MRI-conditioned DDDR permanent pacemaker is a type that can be safe to use during an MRI scan.
**Hypoxemia. The average oxygen level in the arteries(pO2) is about 75 to 100 mm Hg. Hypoxemia is any value under 60 mmHg. Oxygen saturation (O2Sat) is the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen. As measured with a pulse oximeter, the average values range from 95% to 100%. Values under 90% are considered low.
*** Extended-spectrum β-lactamase (ESBL) isolates are bacteria that produce enzymes called ESBLs, which can break down certain antibiotics and make them ineffective. Specifically, ESBLs can hydrolyze three and 4-generation cephalosporins and monobactams. They are commonly found in hospitals, long-term care facilities, and the community. In clinical practice, ESBL-producing bacteria are a significant concern because they can cause serious infections such as urinary tract infections, sepsis, and pneumonia, as illustrated in the present case. Treatment of these infections can be challenging because ESBL-producing bacteria often resist many antibiotics, including penicillins, cephalosporins, and carbapenems. Ultimately, the choice of antibiotics depends on the culture sensitivity test, the patient’s comorbidities, and general condition.
****Steroid-induced leukocytosis (i.e., neutrophilic leukocytosis): Leukocytosis is commonly seen in patients receiving corticosteroid therapy. It occurs within a few hours to days after starting treatment. Leukocytes can adhere to the endothelial lining of blood vessels through L-selectins; steroids inhibit the synthesis of L-selectins, causing the release of neutrophils from endothelial cells into circulation (demargination, 60%). Steroids also down-regulate endothelial molecules like ICAM-1 and PECAM-1, keeping leukocytes in circulation rather than transmigration into tissues. The extent of steroid-induced leukocytosis is usually mild to moderate, rarely exceeding 20,000/cu.mm). Steroid-induced leukocytosis lacks a left shift (toxic granulation) seen in infection. In infection, unsegmented (band) neutrophils are released from the bone marrow, causing the left shift in the WBC count. With a change to the left, there is an increase in band neutrophils and associated lymphopenia, eosinopenia, and monocytosis. A shift to the left indicates an intense or severe inflammatory response. In most cases, steroid-induced leukocytosis is benign and transient, and it resolves once the corticosteroid treatment is discontinued. However, if the leukocytosis persists or is associated with other symptoms, further evaluation may be needed to rule out other causes, such as leukemia.
*****Typical atrial flutter is associated with a re-entry circuit that depends on the inferior vena cava–tricuspid isthmus (CTI) (counterclockwise or clockwise rotation). If the CTI is not involved, it is called “atypical” AFL. This type of AFL can affect any region of RA or LA. In typical AFL, the flutter waves in the inferior leads (II, III, and aVF) and lead V1 are often disconcordant, whereas in atypical AFL, flutter waves are concordant. Catheter ablation is much easier in typical than in atypical AFL.
Keywords:
chronic obstructive pulmonary disease, interstitial pulmonary
disease, pneumoconiosis
UpToDate:
Approach to the adult with interstitial lung disease: Clinical
Evaluation
COPD exacerbations: Management

A 67-year-old woman experienced progressive dyspnea with PND and leg edema for two weeks. PMH was significant for chronic hypertension for 20 years.
This 35-year-old male was transferred from a local hospital for further evaluation after a biopsy of a hard, 4 cm in diameter lymph node in

This 75-year-old man came to the Emergency Department (ED) complaining of abdominal pain for one day. He claimed he had constipation for several months, for
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.