Case 12
A 73-year-old woman, s/p ICD implanted for recurrent ventricular tachycardia (VT) associated with dilated cardiomyopathy (DCM) 9 months ago, was admitted after receiving several electrical shocks.
A 58-year-old man, who had been in good health, became infuriated after a quarrel with his wife for 20 minutes. He suddenly experienced severe chest tightness with breathing difficulty and collapsed. After resuscitation, he was brought to Emergency Department, where he was found to be in a delirious state with laborious breathing. He was afebrile (BT 35.8 °C). BP measured 122/74 mmHg, PR 33/min, and RR 28/min. He was intubated for assisted breathing, followed by transvenous insertion of a temporary pacemaker because of a complete A-V block shown on the ECG. Reportedly, one week before admission, he did have a “cold,” for which he took analgesics for muscle aches. He had no sore throat, fever, chills, or skin rash and had no recent travel. There were no abnormal focal neurological signs. Complete blood counts were normal. Notably, BNP was 475 (N <100) pg/mL, and serum cardiac and liver enzymes were elevated (CK-MB 21.3 [N <5] ng/mL, Tn-I 3.77 [N <0.5] ng/mL, SGOT 183 [N 0-40] U/L, SGPT 109 [N 0-40] U/L). BUN and Cr were 20.9 [6.7-21.3] and 1.8 [N 0.4-1.4] mg/dL, respectively, and eGFR 41.84 ml/min. Serum Na was 133 (N 134-148) mEq/L and K 3.3 (3.4-4.8) mEq/L. The chest X-ray showed normal cardiac size with increased lung markings, suggesting mild pulmonary congestion. Subsequently, cardiac catheterization revealed normal coronary arteries alongside a slightly dilated, globally hypokinetic LV (EF 39.81%). Echocardiography showed impaired LV contractility with global LV hypokinesis (LV EF 39.81). He gradually regained consciousness, and repeated echocardiography revealed preserved LV contractility (LV EF 65%) and diastolic dysfunction after three weeks of hospitalization. However, he had remained in complete AV block throughout and was discharged with a permanent pacemaker.
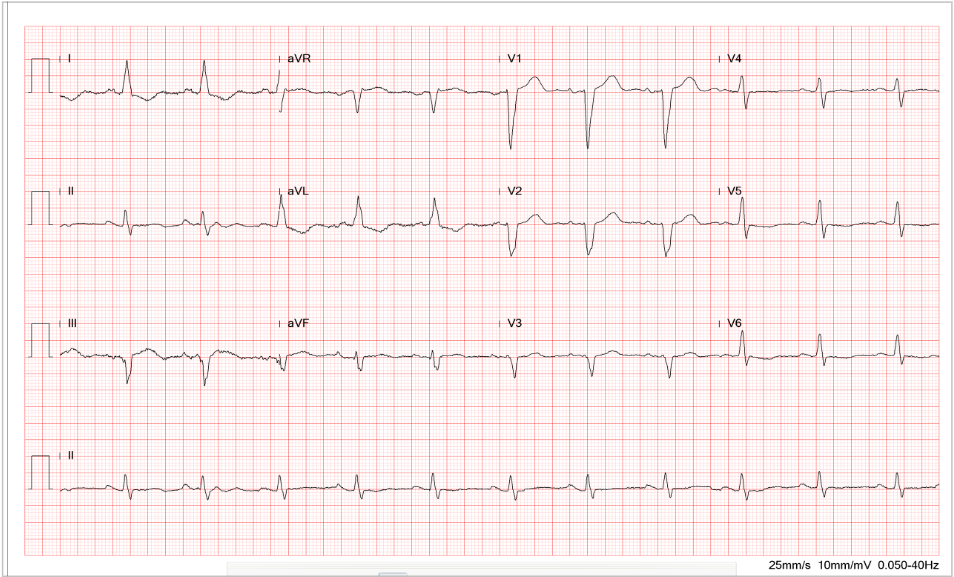
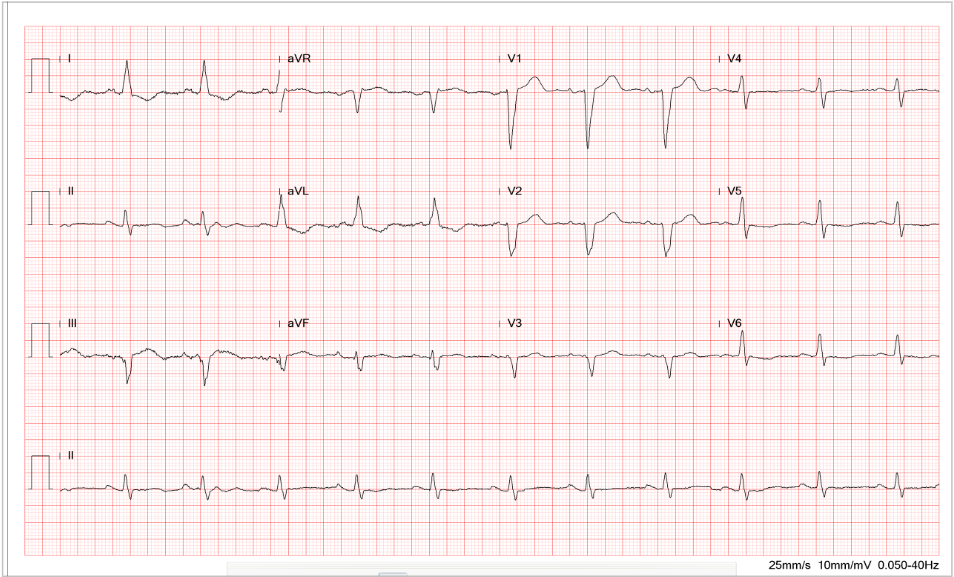
Sinus or atrial tachycardia at 150/min
Complete A-V block (none of the atrial impulses being transmitted to the ventricle; atrial rate 150/min and ventricular rate of the two ventricular escape rhythms 35-45/min.)
Alternating ventricular escape rhythms, one exhibiting negative QRS deflection (rate: 45/min) and the other positive (rate: 35/min) in the lead II
(Due to a lack of sinus-conducted beats, myocardial ischemia/infarction cannot be ascertained.)
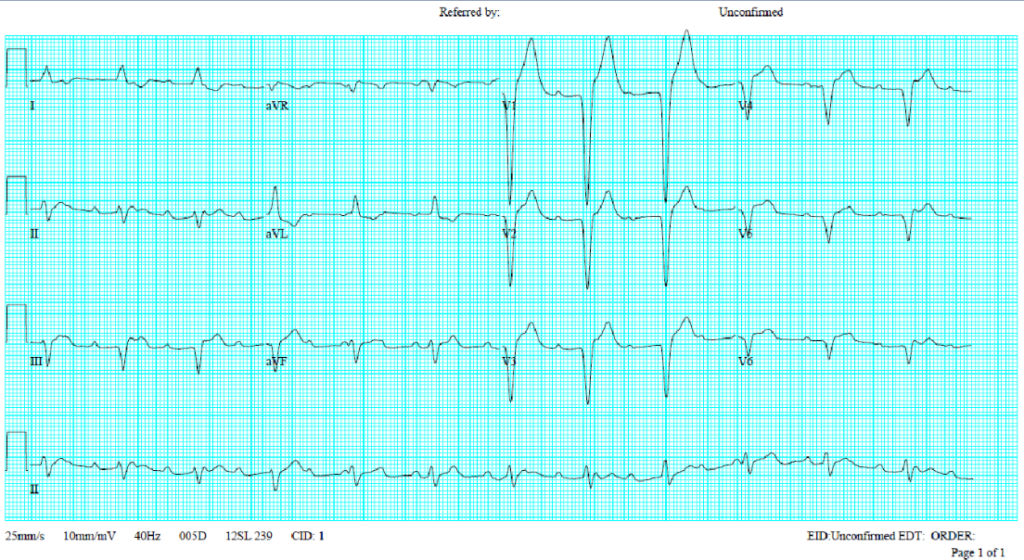
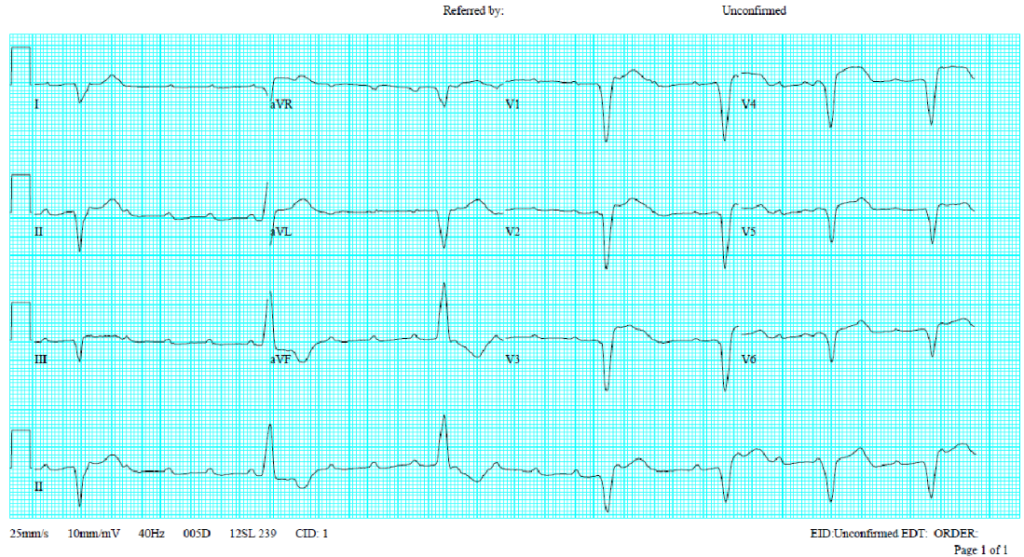
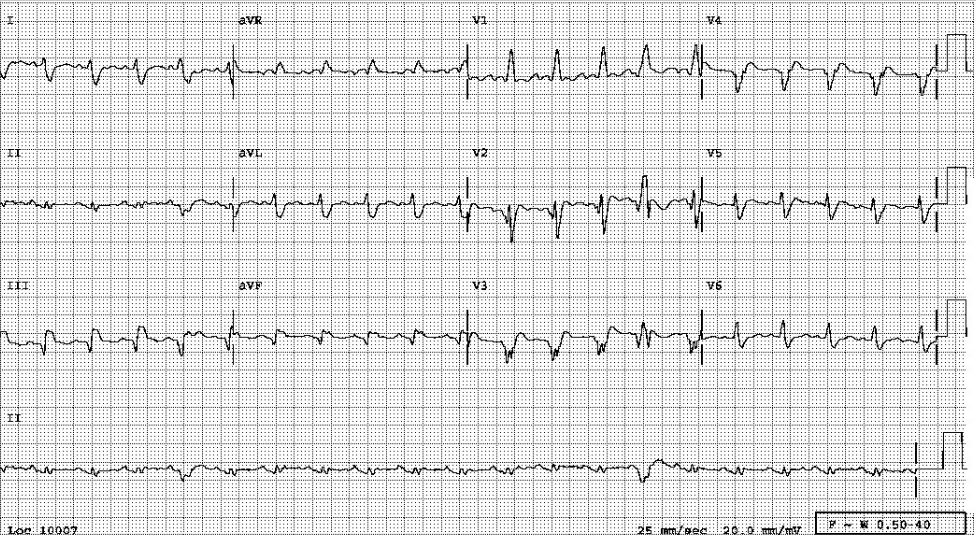
Sinus or atrial tachycardia at 160/min
Complete A-V block (none of the atrial impulses being transmitted to the ventricle; atrial rate 160/min and ventricular rate [the ventricular escape rhythm] 75/min.)
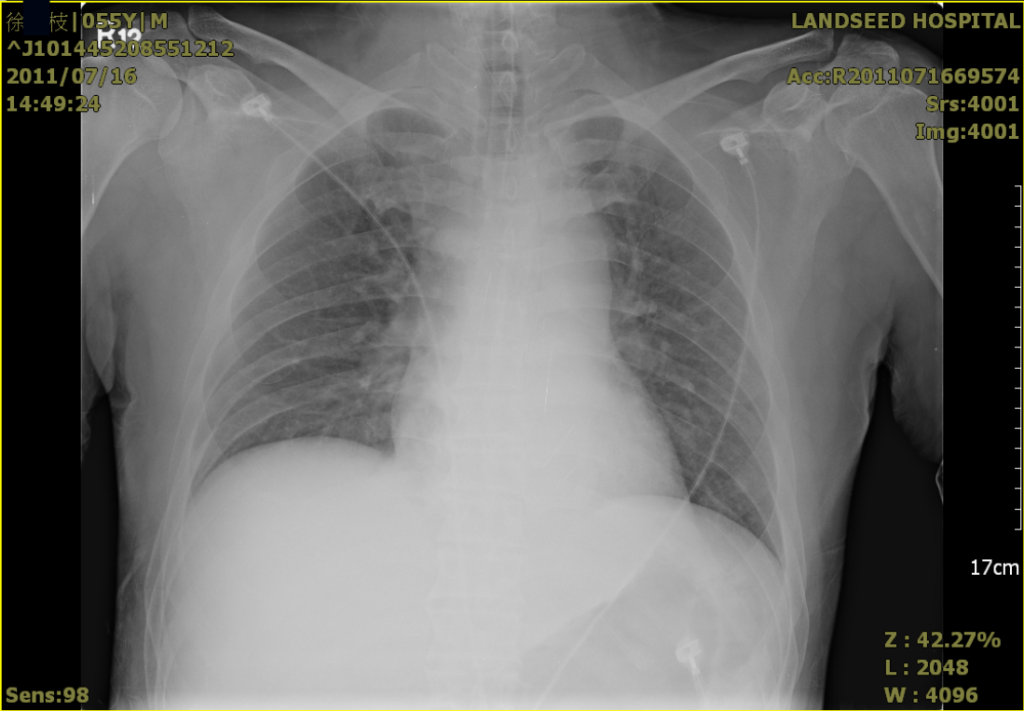
An endotracheal tube in place.
Increased lung markings suggestive of mild pulmonary congestion.
No cardiomegaly.
Concerning the cause of the complete A-V block,* it can only be speculative. While coronary angiography shows no evidence of an atherosclerotic coronary heart, MRI is needed to rule out acute myocarditis. Based on the sequence of events described in the present illness, Takotsubo or stress-induced cardiomyopathy (broken heart syndrome; apical ballooning syndrome) due to catecholamine-induced myocardial toxicity is the likely diagnosis. It is like pheochromocytoma, acute brain injury (e.g., subarachnoid hemorrhage), coronary artery spasm, or dysfunctional microcirculation resulting in myocardial stunning.
Other causes of complete AV block can be physiologic and pathophysiological, including increased vagal tone, fibrosis and sclerosis of the conduction system, ischemic heart disease, cardiomyopathy and myocarditis, congenital heart disease, familial AV block, hyperkalemia, malignancies, neonatal lupus syndrome, hyper- or hypothyroidism, trauma, degenerative neuromuscular diseases; iatrogenic, including, drugs, cardiac surgery, catheter ablation of arrhythmias, alcoholic septal ablation for hypertrophic cardiomyopathy.
Takotsubo cardiomyopathy occurs more commonly in women than men. It may present like acute coronary syndrome with STEMI, Subendocardial MI or QT prolongation, heart failure, tachyarrhythmias (e.g., VT, VF), bradyarrhythmia (including high degree and complete A-V block), sudden cardiac arrest, cardiogenic shock (i.e., hypotension, abnormal mental status, cold extremities, oliguria, or respiratory distress). It may atypically affect the basal portion or whole heart (global hypokinesis).
Differential diagnosis should also include a progression of chronic conduction system disease, autoimmune diseases, adverse effects of certain drugs (e.g., cocaine), infectious diseases, etc. Among infectious diseases, Lyme disease (caused by a species of Gram-negative bacteria of the spirochete class of the genus Borrelia. B. burgdorferi), which not infrequently produces complete AV block, has been reported in Taiwan.
The laboratory findings of multiple organ injury (heart, liver, kidney, etc.) and hypokalemia align with those seen after cardiac arrest and cardiogenic shock.
*Complete A-V block is likely caused by severe ischemia or infarction affecting the A-V junctional area where the A-V node-His bundle resides during cardiogenic shock. If the complete A-V block had recovered, it might show a STEMI ECG pattern in Takotsubo cardiomyopathy.
Keywords:
atrioventricular block, Lyme disease, ST-segment elevation myocardial infarction (STEMI), Takotsubo cardiomyopathy
UptoDate:
Clinical manifestations and diagnosis of stress (takotsubo) cardiomyopathy
Clinical manifestations of Lyme disease in adults
Major causes of atrioventricular block
A 73-year-old woman, s/p ICD implanted for recurrent ventricular tachycardia (VT) associated with dilated cardiomyopathy (DCM) 9 months ago, was admitted after receiving several electrical shocks.

Case 34 Content When this 78-year-old man walked into the clinic, he looked weary and depleted. For the past two days, he had been battling an intermittent fever topping 37.8°C, accompanied by a vanis
A 38-year-old man was admitted because of having abdominal fullness associated with progressive SOB (PND and orthopnea) for ten days. He denied having abdominal pain, chest pain/tightness, fever, cough, or palpitations.
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.