
Case 7
An 83-year-old woman was transferred to Emergency Department (ED) from a local hospital because of a marked deterioration of general status while being treated with
This 43-year-old woman was rushed to ER because of the sudden onset of substernal chest tightness accompanied by cold sweats, which lasted more than 30 minutes. Past medical history (PMH) was significant for hyperlipidemia for five years, excision of retroperitoneal leiomyosarcoma, along with segmental colectomy and total hysterectomy without evidence of tumor metastasis six years ago, and s/p radiotherapy and chemotherapy for stage IV leiomyosarcoma involving the spleen, right pelvic wall, and cardiac right ventricle (RV)as detected by CT scan two years ago. One month prior, she also had duodenal bleeding due to tumor metastasis. Her family history was positive for atherosclerotic coronary heart disease (CHD) (mother 65 and two brothers in their 40’s). On arrival, she appeared obese (BMI 31.1), pale, and in respiratory distress. BP measured 120/75 mmHg, PR 102/min (regular), and RR 25/min. There was no jugular venous distension. Heart sounds were distant, and PMI was not visible, but a grade 2/6 systolic murmur was audible along the left 2nd and 3rd sternal border. Lungs were clear. The abdomen showed previous surgical scars. Laboratory data revealed Hb 9.9 g/dL, Plt 196 K/uL, WBC 21,230/uL with 87% Neu, INR 1.07, and Troponin-I 0.01 ng/mL, CK-MB 2.3 U/L, BUN 12 mg/dL and Cr. 0.86 mg/dL. ECG exhibited ST-segment elevation and T wave inversion in V1-V4 alongside intraventricular conduction defect (IVCD), suggesting acute myocardial infarction involving the proximal left anterior descending artery (LAD). Accordingly, the care team prompted cardiac catheterization with coronary angiography; It revealed insignificant CHD, i.e., except for 30% occlusion in LCX, LM, LAD, and RCA were patent. However, LAD and RCA notably supplied blood to an ill-defined, highly vascularized RV mass. Echocardiography estimated the RV tumor to be 2-3cm in thickness, extending from the RV apex to the RV outflow tract (RVOT)(confirmed by CT scan), which protruded into the pulmonary artery during the systolic phase, causing mild and pulmonary stenosis. The ECG ST-segment elevation in V1-V4 resolved after supportive hydration therapy. Under the diagnosis of acute coronary syndrome presumed to be due to a coronary artery steal phenomenon related to an RV metastatic leiomyosarcoma, the care team consulted the oncology and surgical specialists.
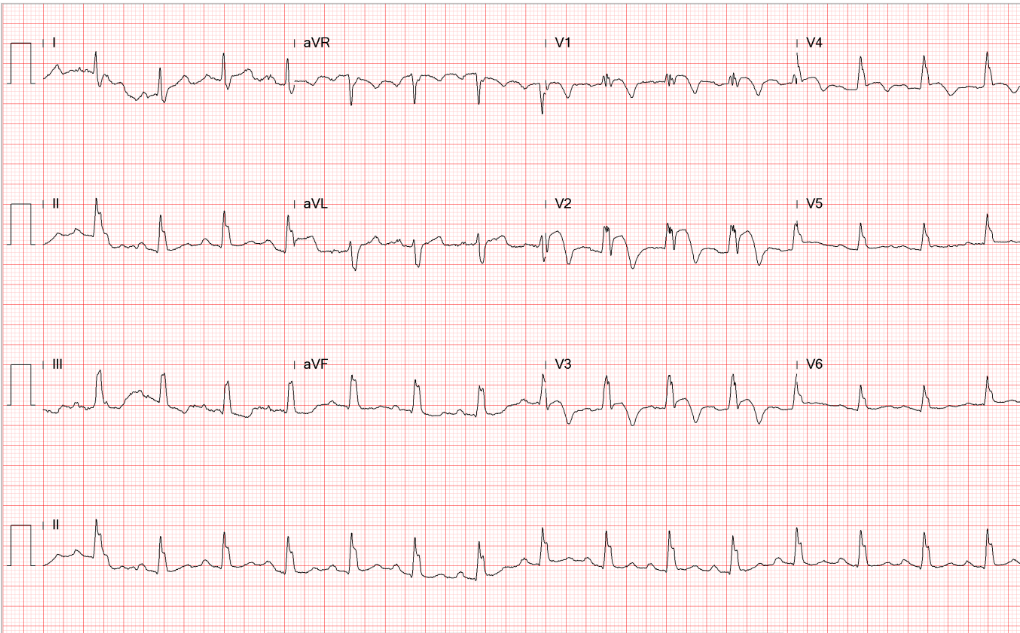
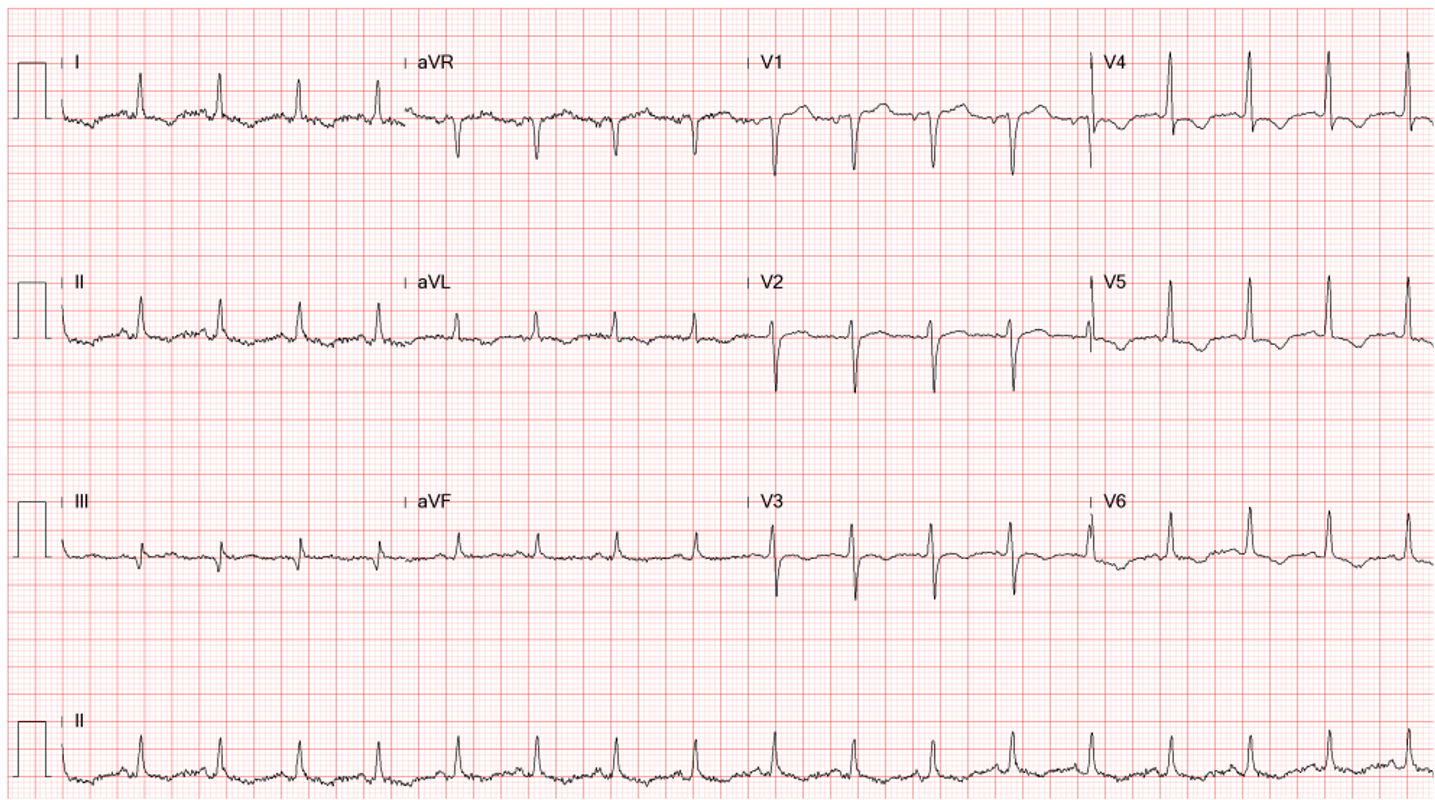
Sinus rhythm at 95/min.
Intraventricular conduction defect (IVCD) (QRSd 110 msec)
ST-segment elevation and T wave inversion in V1-V4 suggestive of acute myocardial infarction
Tall R wave in V1-V4 (clockwise rotation) r/o RVH
(Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)
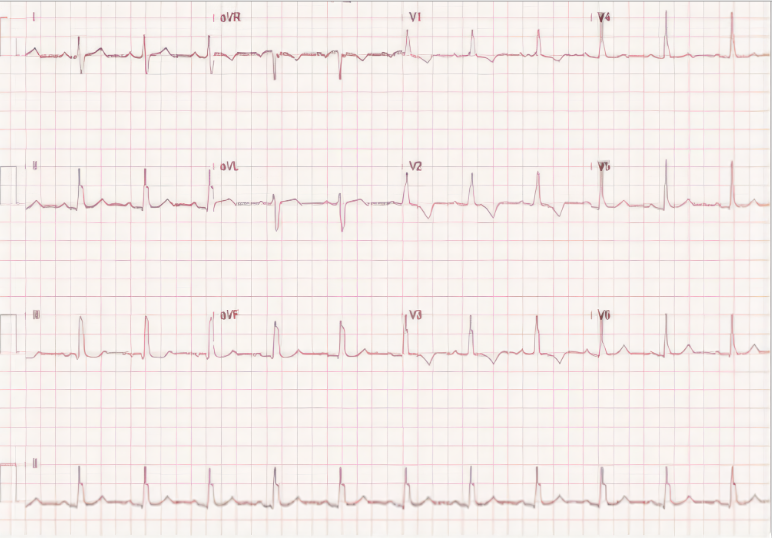
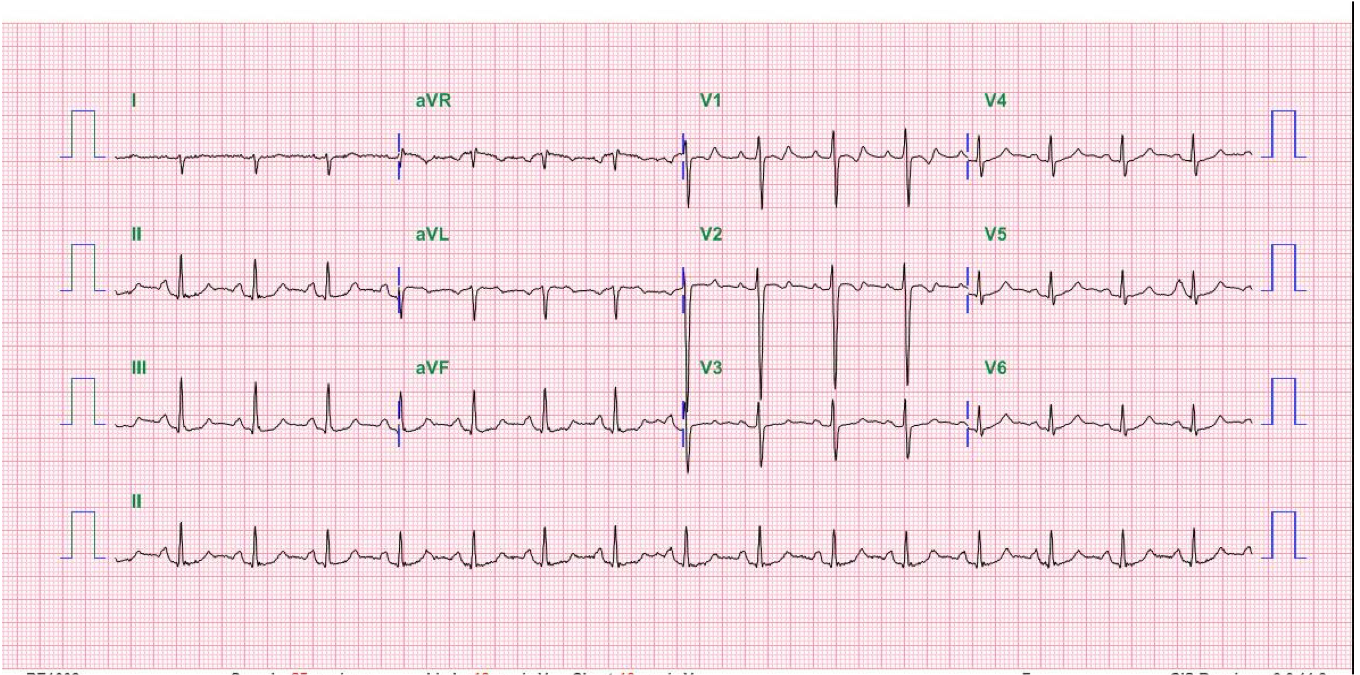
ST-segment elevation and T wave inversion in V1-V4, but not IVCD, resolved after supportive hydration therapy.
The increase in the R wave amplitude may be positional.
(Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)

Obesity
s/p EKG lead placement. s/p port A catheter placement, right
Torturous aorta with atherosclerotic change
Borderline cardiomegaly.
Numerous opacities in regressive (faint) appearance at the bilateral lung fields, compatible with lung metastasis.
(Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)
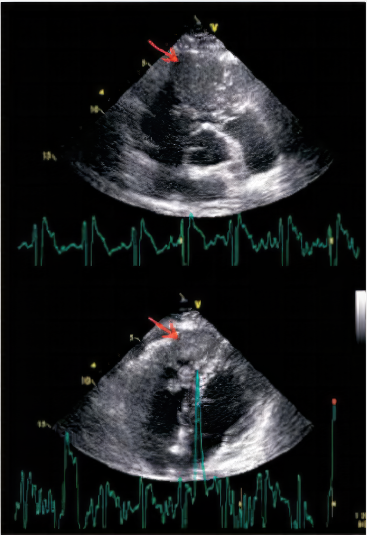
The parasternal short-axis view (Top) and apical four-chamber view (Bottom) showed an ill-defined, lobulated mass (thickness: 2~3cm) over the RV apex to RV outflow tract (RVOT) (arrow). It protruded into the pulmonary artery during the systolic phase, causing mild and pulmonary stenosis. LV systolic function is preserved, and LV and LA are not dilated.
(Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)
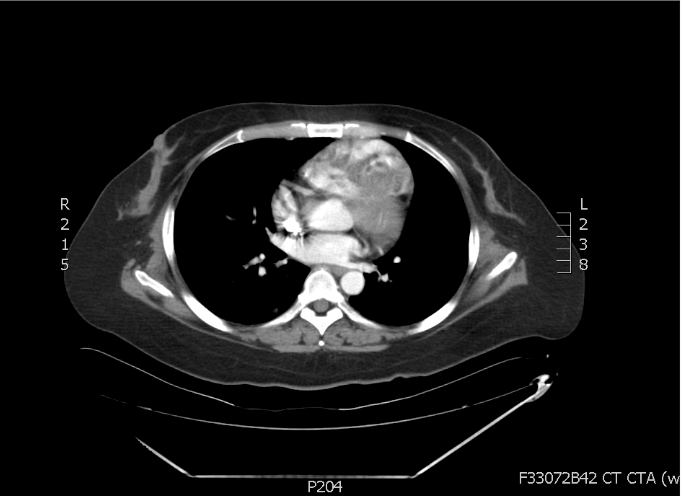
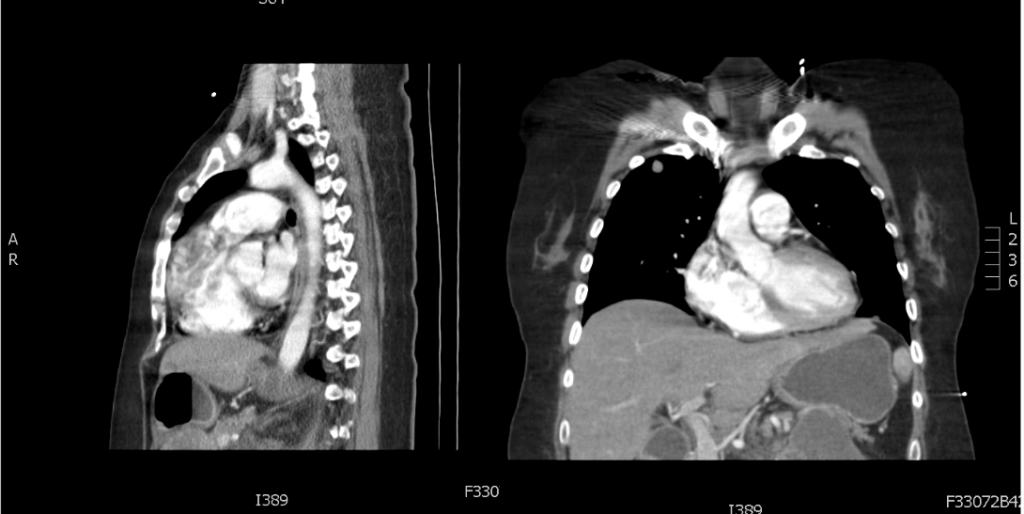
An ill-defined soft tissue mass with ventricle septal involvement (arrow). (Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)
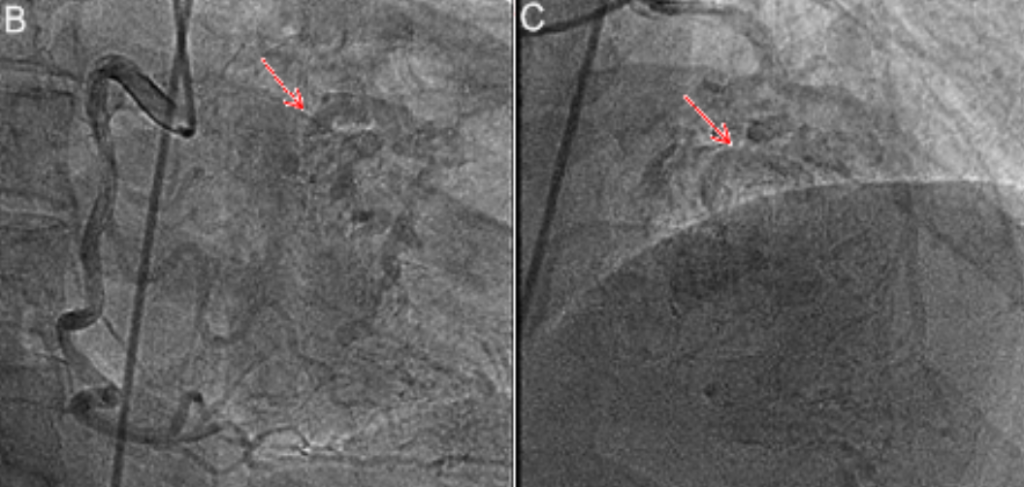
B (Left). Right coronary artery (RAO caudal view) and C (Right): Left anterior descending artery (RAO cranial view) showed coronary patent coronary lumen with additional flow to a vast and ill-defined myocardial mass lesion (arrow). Overall, LM: patent; LAD: patent, shunt to RV mass; LCX: 30% stenosis at the distal; RCA: patent, shunt to RV mass. (Permission granted by Acta Cardiologica Sinica, Taipei, Taiwan)
The ECG finding of ST-segment elevation in V1-V4 in association with chest tightness of sudden onset should arouse the suspicion of acute coronary syndrome (ACS) with STEMI despite the lack of cardiac enzyme elevation. The PMH of hyperlipidemia and family history of premature atherosclerotic CHD (younger than 45) further support the diagnosis. The ECG presence of IVCD (i.e., RBBB, LBBB, or nonspecific QRS morphology in the present case) suggests the culprit lesion could be very proximal at the LAD before the take-off of septal perforators, which provide blood supply to the His-Purkinje system. Admittedly, IVCD can be due to a separate chronic process (e.g., chronic conduction system disease) unrelated to CHD.
The coronary angiography’s unveiling of an RV mass receiving blood supply through shunting from LAD and RCA is astonishing. It is intriguing that despite chemotherapy two years prior, the RV tumor has grown progressively to gain blood supply from these coronary arteries. The differential diagnosis in highly vascularized cardiac tumors should include angiosarcoma or hemangioma. Shunting blood supply from LAD and RCA to a tumor can cause a coronary steal phenomenon, and thus type 2 myocardial ischemia* leading to angina pectoris and even MI. Under this circumstance, the possibility of coronary artery embolization causing STMI should also be entertained.
The ischemic process seems acute and transient as the ST-segment elevation resolves after supportive hydration therapy. However, a chronic ischemic process involving the interventricular septum is likely present because of the coronary steal phenomenon. Chronic ischemia of the septum can induce fibro-degenerative changes resulting in chronic IVCD. Alternatively, the RV tumor can infiltrate the ventricular septum, directly damaging the His-Purkinje system, causing conduction disturbance, and even complete heart block.
Cardiac tumors, either primary or secondary, are rare. Metastatic involvement of the heart, as in the present case, is more common than primary cardiac tumors like atrial myxomas, fibroelastomas, etc. Cardiac tumors inducing a coronary steal phenomenon causing angina or ACS, as in the present case, have been scantly reported in patients with cardiac tumors (e.g., atrial myxoma). Otherwise, signs and symptoms of cardiac tumors can usually come from four different mechanisms: constitutional (rarely, e.g., fever, anemia associated with atrial myoma), embolic (i.e., pulmonary or systemic embolization due to blood clots and tissue debris on the surface of the tumor), infiltrative (esp. LV tumors, causing arrhythmias and conduction defect, and pericardial effusions with or without tamponade), and obstructive (e.g., pulmonary stenosis, tricuspid regurgitation, right-sided HF; mitral stenosis, mitral regurgitation, left-sided HF). Sudden cardiac death can result from either an RV or LV tumor. Timely use of echocardiography, MRI, and CT scan can quickly confirm the diagnosis.
Surgery can easily ligate and transect the feeder vessels and resect benign but not malignant cardiac tumors. After resection for imminent obstructive symptoms, malignant tumors often require chemotherapy and irradiation therapy; a complete cure is unlikely, as illustrated in the present case, and the prognosis is grim.
*Type 2 myocardial ischemia: Myocardial ischemia is caused by a mismatch between oxygen supply and demand with or without CHD rather than that (type 1) with CHD precipitated by atherosclerotic plaque disruption (rupture or erosion).
Keywords:
cardiac tumors, coronary steal phenomenon, intraventricular conduction defect (IVCD), type 2 myocardial infarction
UpToDate: Cardiac tumors
Satoshi Takenaka et al. Eleven Cases of Cardiac Metastases from Soft-tissue Sarcomas
Jpn J Clin Oncol 2011;41(4)514–518
Abbas Agaimy et al. Primary and metastatic cardiac sarcoma: a 12-year experience at a
German Heart Center Int J Clin Exp Pathol. 2012;5(9):928-38
Tam Weng-Chio et al. Right ventricle mass induced coronary artery steal phenomenon: A rare
clinical manifestation on one leiomyosarcoma patient. Acta Cardiol Sin 2015;31:464E467.

An 83-year-old woman was transferred to Emergency Department (ED) from a local hospital because of a marked deterioration of general status while being treated with
This 50-year-old man came to the Emergency Department complaining of having substernal chest pain for more than 10 hours. The pain was sharp and not
A 52-year-old man was admitted because of progressive dyspnea on exertion for one week. In the past, he had chronic obstructive pulmonary disease (COPD), alcoholic
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.