
Case 6
A 35-year-old woman with Marfan syndrome presented with increasing dyspnea, fever, productive cough, and chest tightness for one day.
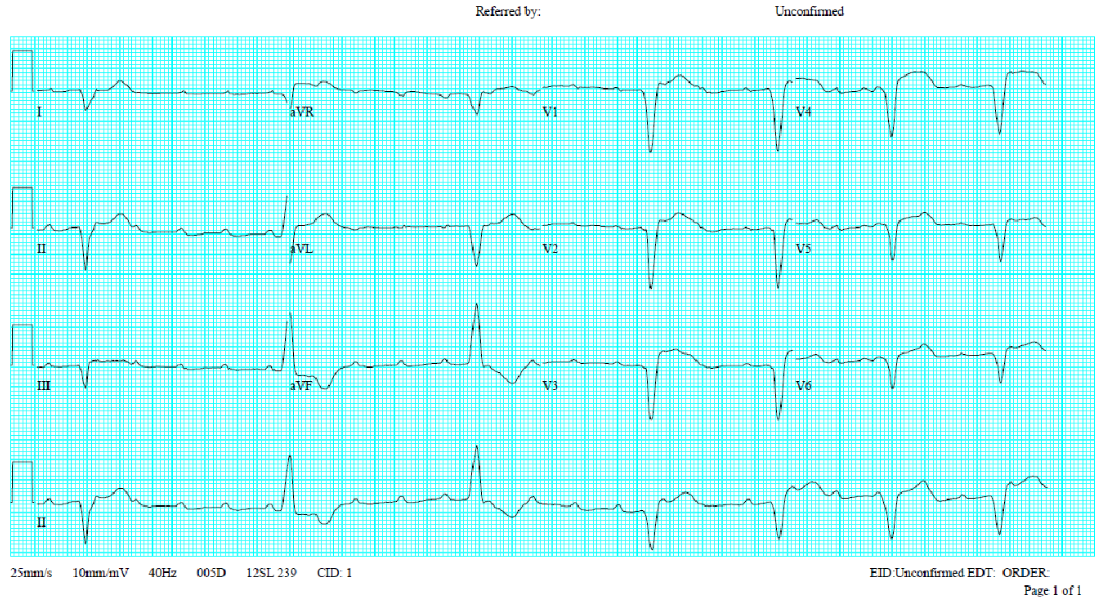
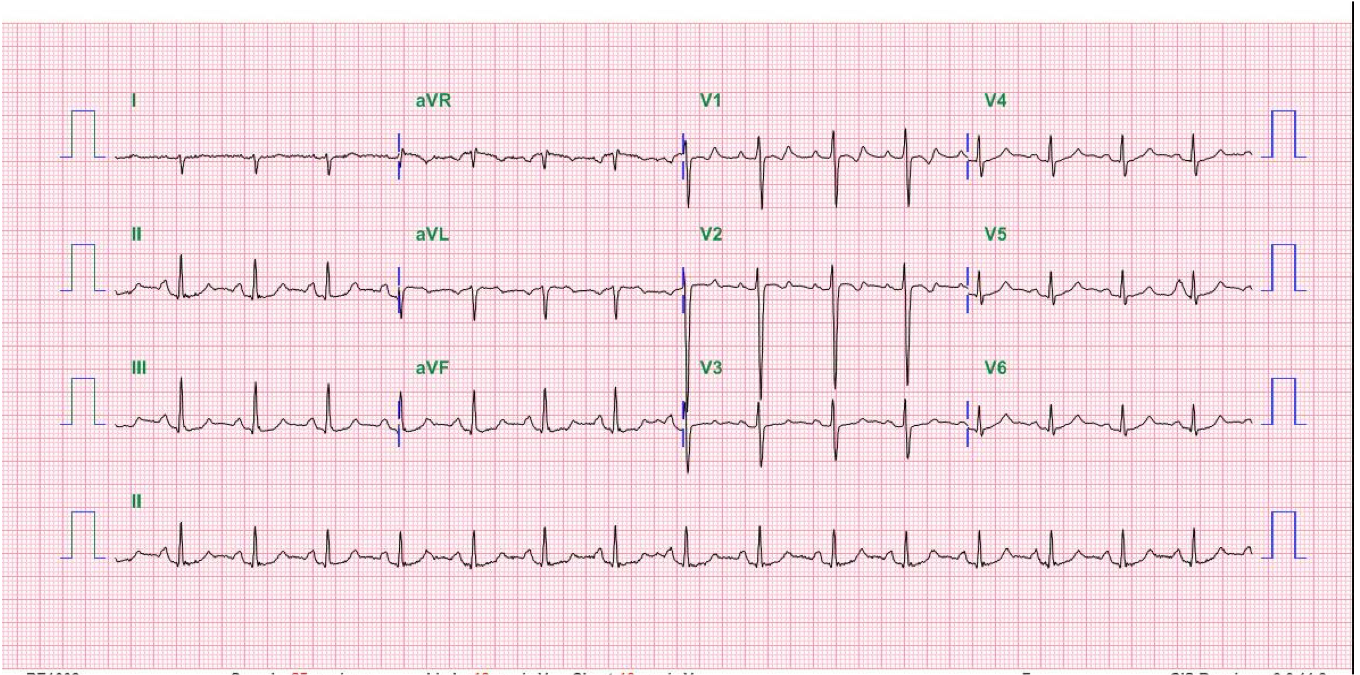
A 72-year-old woman, who had been in the hospital for treatment of right leg cellulitis for two days, suddenly developed increasing SOB with worsening heart failure (HF) 6 hours after a blood transfusion of 2 units packed cells for chronic anemia (Hb 7.8 mg%) (Chest X-ray 1 and Chest X-ray 2). PMH was significant for chronic HF relating to hypertensive cardiomyopathy, chronic atrial fibrillation (AF), and end-stage renal disease (ESRD), presumably nephrosclerotic (BUN 125 mg/mL, Cr 8.8 mg/mL, and eGFR 5 ml/hr). Physical findings were consistent with biventricular HF- PMI displaced to the left, RV and LV lifts, a Gr 2/6 systolic murmur at the apex and left sternal border, loud S3 gallop, and bilateral crackles at both lung fields. BT measured 38.1°C, BP 177/84 mmHg, PR 130/min, irregular, and RR 20/min. Jugular veins were distended with JVP measured 10 cm H2O. In addition to cellulitis of the right leg, there was 4+ pitting edema in both legs. Corresponding to the worsening HF incurred after blood transfusion, there was newly developed ST depression with T wave inversion in II, III, and aVF. Additionally, there was a rightward shift of the QRS axis (from +74° to +95°) alongside a more clockwise heart rotation with more extent of slow R progression in the precordial leads (ECG 1 before and ECG 2 after blood transfusion). After ruling out acute myocardial infarction (MI) and pulmonary embolism (i.e., no elevation of cardiac enzymes and D-dimer in serial blood sampling), the ECG changes were attributed to blood transfusion-induced volume overload, which resulted in the worsening of HF.
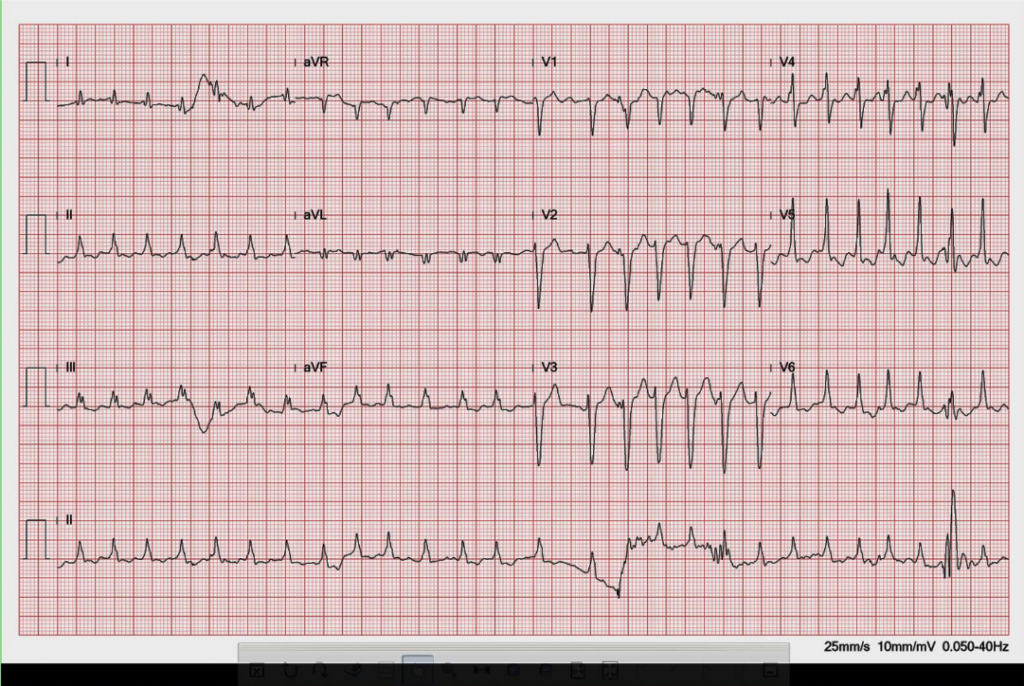
AF with a rapid ventricular rate of 164/min.
Low voltage in limb leads.
Widened QRS (fragmented, IVCD, QRSd 118 ms) with a normal QRS axis (+74°)
Slow progression of R in precordial leads with R/S transition at V4
Q in aVL
LVH or incomplete LBBB pattern (or IVCD)
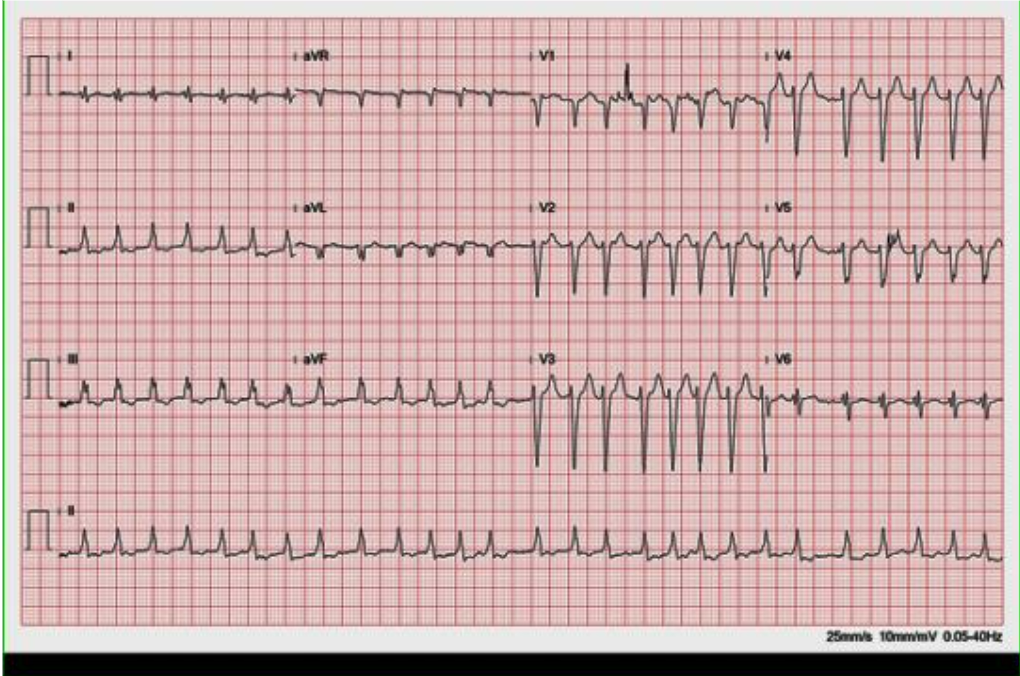
AF with a rapid ventricular rate of 166/min.
Low voltage in limb leads.
Widened QRS (fragmented; QRSd 114 ms) with right AD (+95°) ST depression and T wave inversion in II, III, and aVF
Slow progression of R in precordial leads with R/S transition at V6
Q in aVL
LVH or incomplete LBBB pattern (or IVCD)

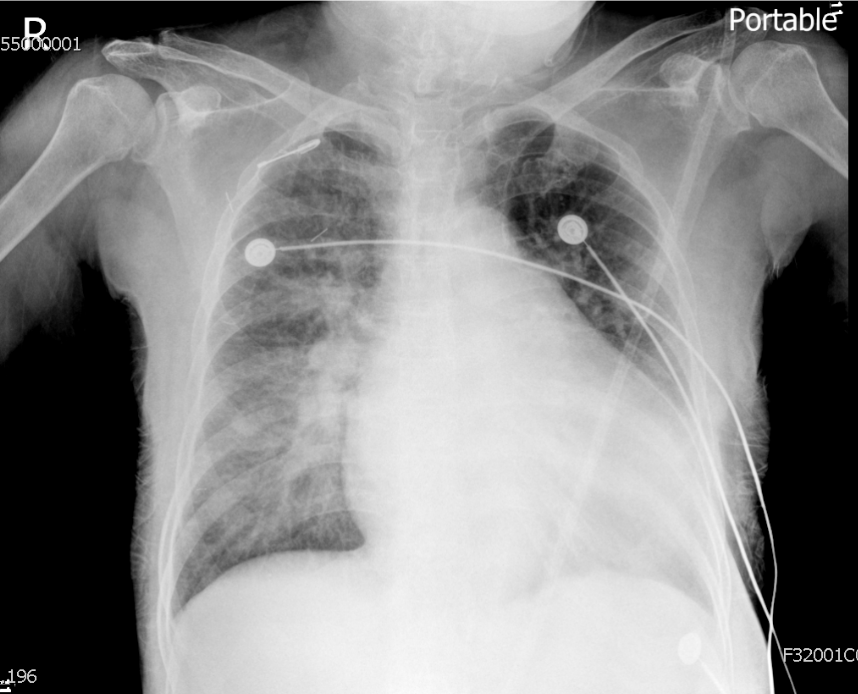
LV and LA enlargement.
Prominent PA suggestive of pulmonary hypertension
Pulmonary congestion with blunting of bilateral costophrenic angles (pleural effusion) – more marked following blood transfusion.
The noted ECG changes, as described above, are likely to reflect volume and pressure overload of RV induced by blood transfusion in the clinical setting of chronic HF and renal failure (ESRD). Clinical triggers for worsening HF that can lead to such ECG changes must be contemplated in all patients. Volume overload is one of the triggering factors that can worsen HF in the clinical setting of chronic cardiac dysfunction. Other factors include but are not limited to medical noncompliance, dietary indiscretion, deterioration of renal function, acute myocardial ischemia/infarction, pulmonary embolism, anemia (acute and chronic), infection (e.g., pneumonia, endocarditis), the onset of tachyarrhythmias such AF, SVT, VT, or severe bradycardia, endocrine disorders (e.g., hyperthyroidism), drugs with negative inotropy, etc. Many of these triggering factors are preventable. For instance, as in the present case, blood transfusion can be given after better improvement of HF and better control of the ventricular rate of AF and is immediately followed by diuretic therapy.
Keywords:
atrial fibrillation, blood transfusion, heart failure, end-stage renal disease (ESRD)
UpToDate:
Treatment of acute decompensated heart failure: General considerations
The management of atrial fibrillation in patients with heart failure

A 35-year-old woman with Marfan syndrome presented with increasing dyspnea, fever, productive cough, and chest tightness for one day.
A 58-year-old man, who had been in good health, became infuriated after a quarrel with his wife for 20 minutes. He suddenly experienced severe chest
A 52-year-old man was admitted because of progressive dyspnea on exertion for one week. In the past, he had chronic obstructive pulmonary disease (COPD), alcoholic
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.