
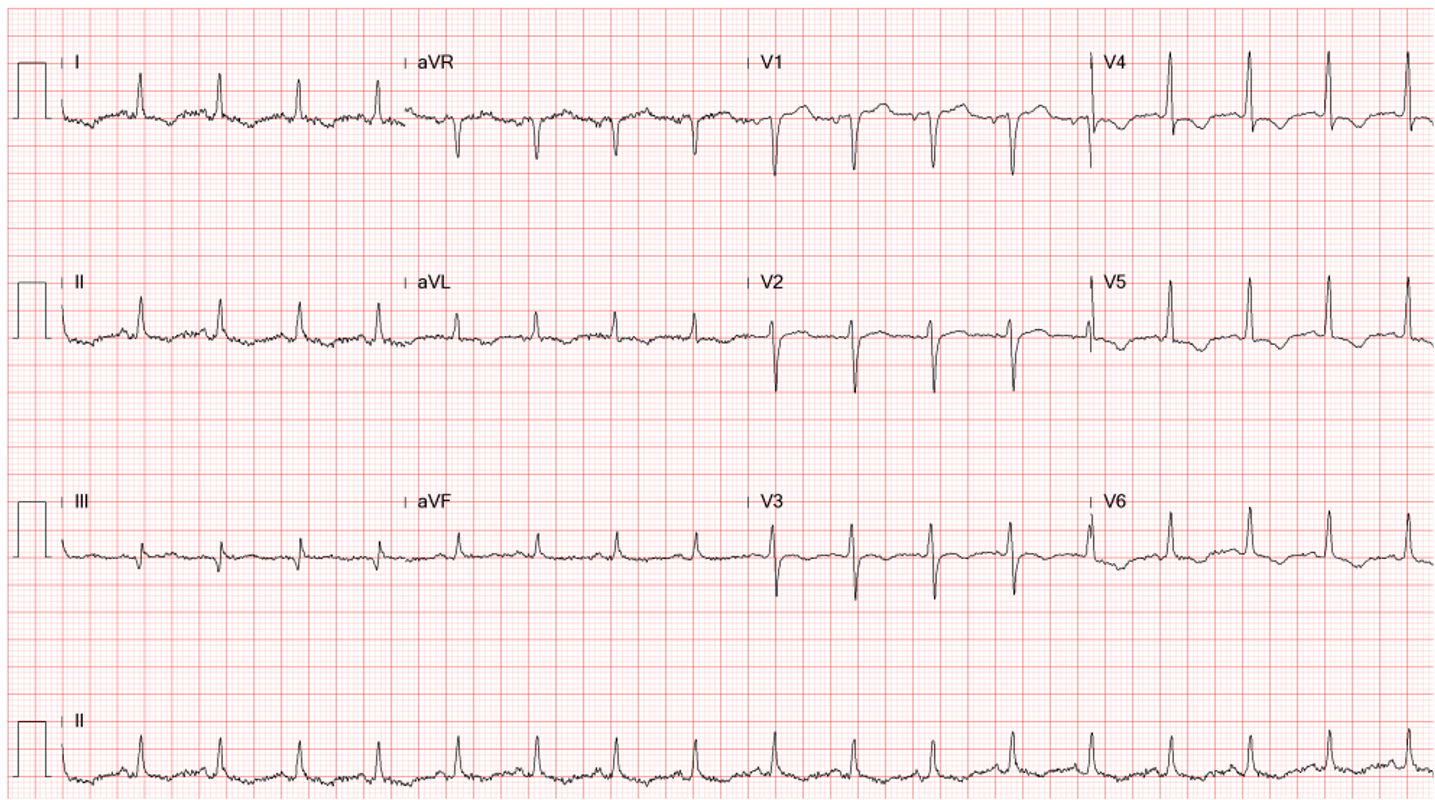
Case 1
A 57-year-old woman with a long-standing history of bronchial asthma and COPD was admitted because of intermittent episodes of dyspnea associated with palpitations and general
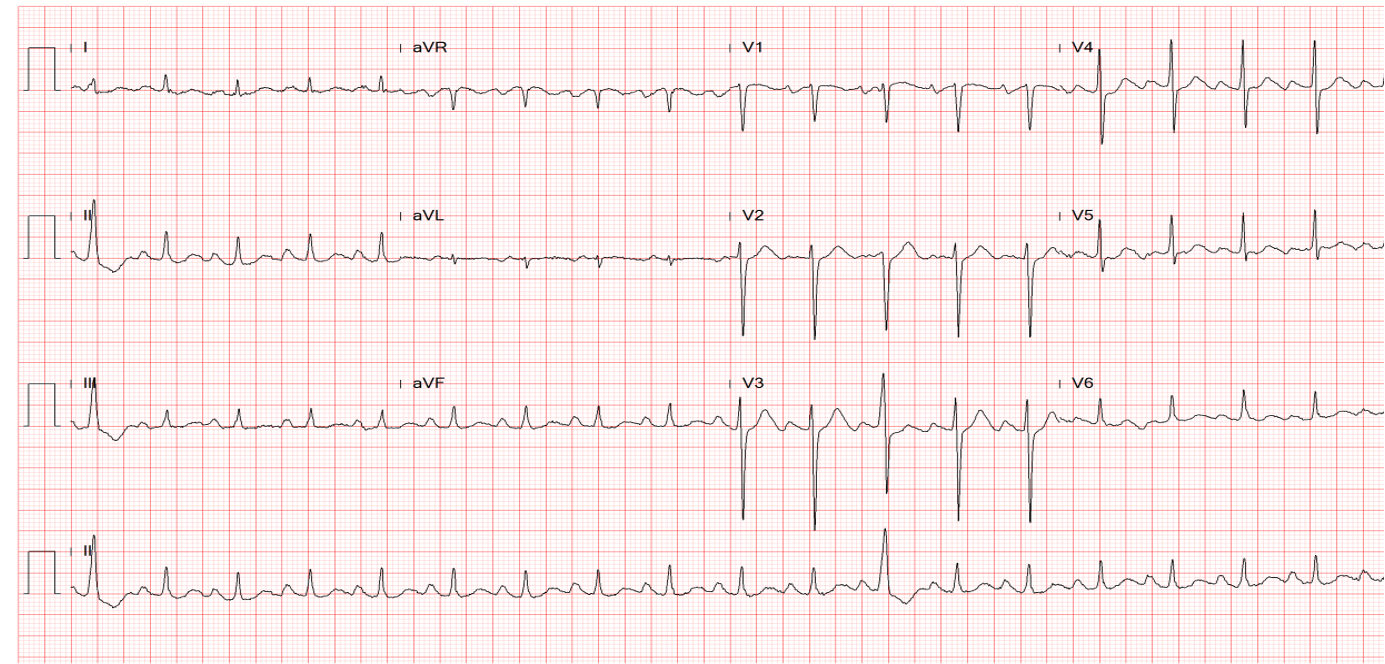
A 62-year-old man was brought to Emergency Department for severe chest tightness of sudden onset, lasting 30 min. He had experienced episodes of chest tightness unrelated to exertion for one year. About one week prior, the frequency of these episodes had increased from 2-3/week to 4-5/week. Past medical history was significant for diabetes mellitus and hypertension for over ten years. He also had TIA about one year ago. He had been on peritoneal dialysis for one and a half years due to end-stage renal disease (ESRD), presumably related to diabetic nephropathy. On physical examination, he was afebrile, obese, and in no respiratory distress. BP measured 110/70 mmHg, PR 80/min, and RR 16/min. Except for a loud S4, cardiac and pulmonary findings were unremarkable. ECG showed ST depression in I, II, III, aVF, and V2-V6, and T inversion in III, aVF, and V3-V6. Notably, there was accompanying ST elevation in aVR ≥ 1mm, suggesting extensive subendocardial myocardial ischemia/infarction (NSTEMI). Hb was 10.8 g/mL, and liver enzymes and electrolytes were within normal limits. Tn-I and CK-MB were elevated within 3 hours after arrival (0.41 to 8.5 [N <0.5] ng/mL and 10 to 21.5 [N <5] ng/mL, respectively). Chest X-ray illustrated obesity with lung markings slightly increased in both lower lung fields. Subsequent cardiac catheterization with coronary angiography revealed preserved LV systolic function and severe triple vessel disease with LM ostium 30-40% narrowing, LAD-mid 100% stenosis, LCX-proximal 80% stenosis, LCX-mid 80% stenosis, LCX-OM1 80% stenosis, RCA-mid 90% stenosis, RCA-PDA 90% stenosis. Based on these findings, following acute management for NSTEMI, surgical consultation for CABG aimed at total revascularization was obtained.
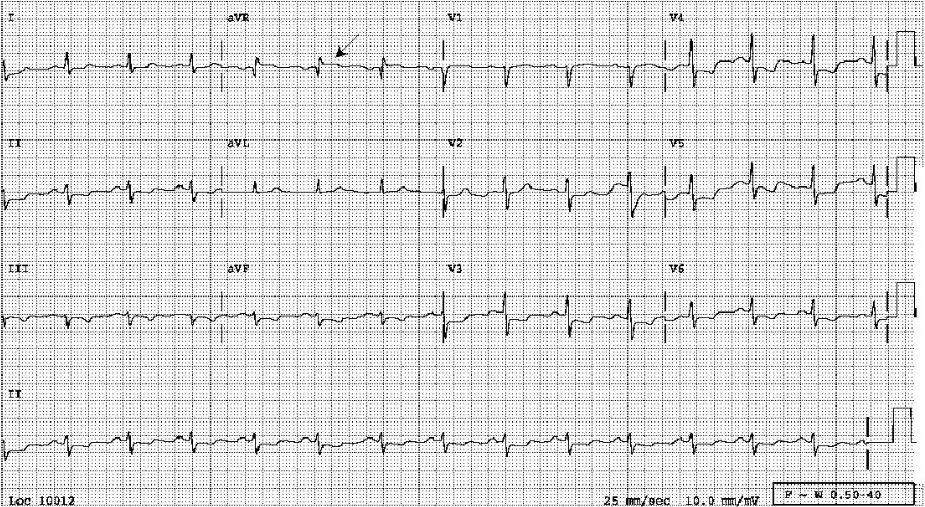
Diffuse low voltage*
Sinus rhythm at 85/min with left AD (-30°)
ST depression in I, II, III, aVF, and V2-V6, and T inversion in III, aVF, and V3-V6.
ST elevation in aVR ≥ 1mm (aVR > V1; arrow), suggestive of diffuse subendocardial myocardial ischemia/infarction (NSTEMI)
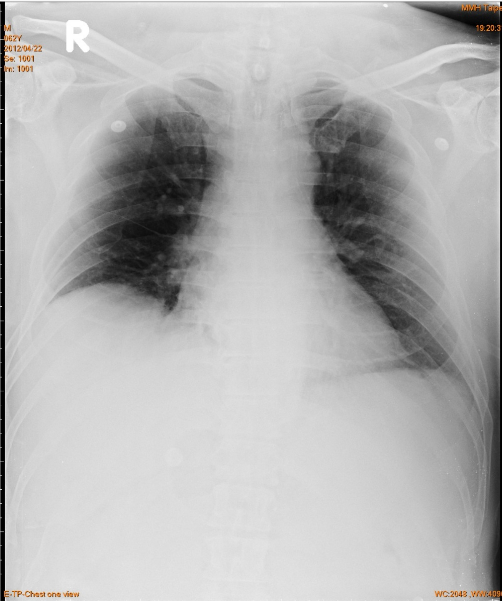
Obesity
Lung markings slightly increased
in both lower lung fields
Clear bilateral costophrenic angles
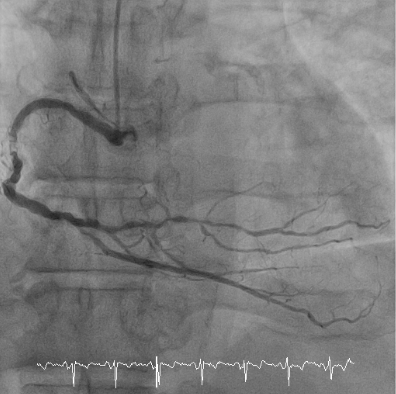
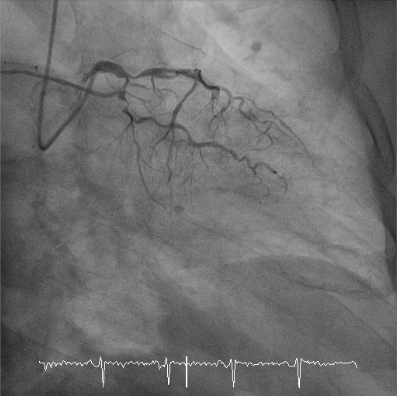
Preserved LV systolic function without significant regional wall motion abnormality (not shown)
LM ostium: 30-40% narrowing; LAD-mid: 100% stenosis; LCX-proximal: 80% stenosis, LCX-m: 80% stenosis, LCX-OM1: 80% stenosis; RCA-m: 90% stenosis, RCA-PDA: 90% stenosis.
Patients with “acute coronary syndrome” may manifest as NSTEMI rather than just unstable angina, as evidenced by the elevation of cardiac enzymes in this case. Notably, diffuse ST depression is accompanied by ST elevation in aVR ≥ 1mm (aVR > V1). These findings suggest the likelihood of atherosclerotic coronary heart disease (CHD) with a significant left main (LM) coronary artery lesion or severe triple vessel disease with or without a proximal left anterior descending (LAD) occlusion.
The limb lead aVR is referred to as the “Cavitary Lead,” vectorcardiographically, opposite to I, II, aVL, and V4-V6; ST elevation in aVR may thus represent a reciprocal change to ST depression in those leads. However, due to the lead placement, ST elevation in aVR may also reflect transmural ischemia/infarction of the basal interventricular septum caused by an occlusive lesion in the proximal left coronary artery system. Furthermore, ST elevation in aVR with ST depression in I, II, aVL, and V4-V6 can also occur in significant hypotension (e.g., cardiogenic shock) and severe myocarditis or cardiomyopathy. Lastly, as shown in the present case, total revascularization with CABG is generally recommended in patients with a significant LM lesion and atherosclerotic triple vessel CHD.
* Causes of low voltage ECG include but are not limited to obesity, COPD, pericardial effusion, progressive cardiac myocarditis, or cardiomyopathy. In this case, diffuse low ECG voltage is due to obesity (see Chest X-ray).
Keywords:
acute coronary syndrome (ACS), atherosclerotic coronary heart disease (CHD), cavitary lead aVR, Non-ST-segment elevation myocardial infarction (NSTEMI)
UpToDate:
Classification of unstable angina and non-ST elevation myocardial infarctionOverview of the acute management of unstable angina and non-ST elevation myocardial infarction
Kosuge M, et al. An early and simple predictor of severe left main and/or three-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Am J Cardiol 2011; 107:495-500.

A 57-year-old woman with a long-standing history of bronchial asthma and COPD was admitted because of intermittent episodes of dyspnea associated with palpitations and general
This 50-year-old man came to the Emergency Department complaining of having substernal chest pain for more than 10 hours. The pain was sharp and not
This 72-year-old man, a retired coal miner with a known history of chronic obstructive pulmonary disease (COPD) and pneumoconiosis, came to the Emergency Department complaining
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.