Case 29
A 56-year-old man came to the Emergency Department because of worsening dyspnea with a productive cough for the past two weeks. Notably, he smoked one
A 38-year-old man was admitted because of having abdominal fullness associated with progressive SOB (PND and orthopnea) for ten days. He denied having abdominal pain, chest pain/tightness, fever, cough, or palpitations. Before admission, the local physician noted elevated liver enzymes with normal AFP and negative hepatitis markers (hepatitis B or C) and splenomegaly on abdominal ultrasound. He was a heavy smoker. Family history was negative for diabetes mellitus but strongly positive for atherosclerotic coronary heart disease (CHD) with prior myocardial infarction (MI) (parents, two brothers, and one sister). On admission, he was moderately obese, afebrile, and mentally alert in moderate respiratory distress (BP 124/77 mmHg, RR 20/min, and PR 106/min). There were physical signs of biventricular heart failure (HF) (JVD with JVP 11 cm H2O, bilateral crackles with percussion dullness at posterior lower 1/3 of the right lung field, PMI shifted to the left, apical S3 and a Gr 2/6 systolic murmur which increased in intensity with inspiration). The ECG showed Q in II, III, aVF, and V2-V4, suggesting inferior and anterior MI of undetermined age. The chest X-ray confirmed cardiomegaly, and echocardiography showed marked LV enlargement and global LV hypokinesis (LVEF 25%) with regional wall motion abnormalities in anteroseptal, apical and inferior segments, moderate MR, and severe TR. Pertinent laboratory data included Hb 14.1 g/dL, WBC 12,100 /uL, BNP, 1780 (N: 400) pg/mL, Tn-I: 0.92-0.76 [N <0.12] ng/mL, CK-MB: 1.9 [N <5.0] ng/mL, Alk-phosphatase 94 IU/L, ALT(GPT): 469 IU/L, BUN 15 mg/dL, Cr. 1.2 mg/dL, AST(GOT): 138 IU/L. Elevation of liver enzymes was attributed to liver congestion as they declined following the improvement of HF. Because the critical time window (counting from the onset of symptoms) had passed, the care team deferred primary PCI. After treatment of HF, subsequent coronary angiography revealed severe triple vessel atherosclerotic CHD (LAD: total occlusion, LCx-distal: 70% stenosis; LCx-OM1: total occlusion, RCA-Mid: total occlusion, collateral circulation: LCx collateral to LAD and RCA). Accordingly, the patient was referred for surgery (i.e., CABG for complete revascularization).
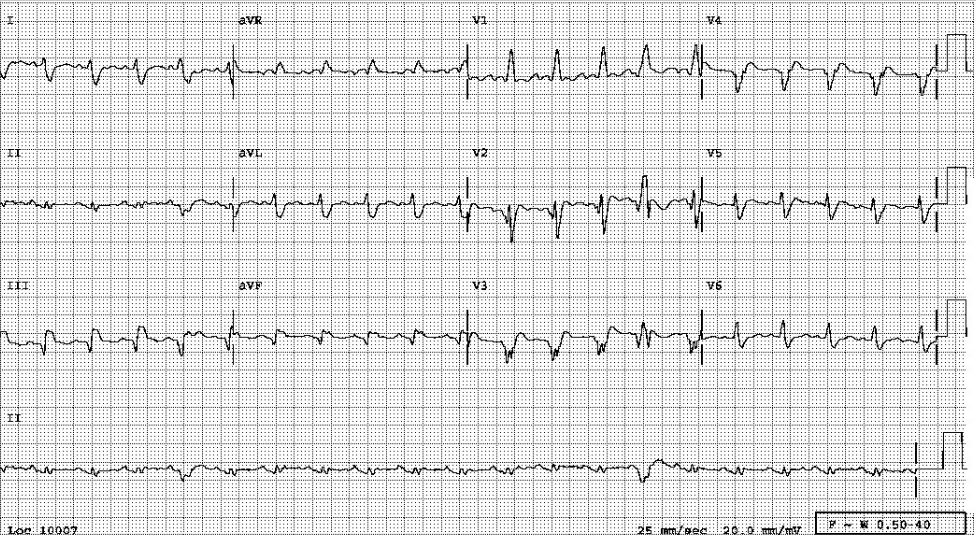
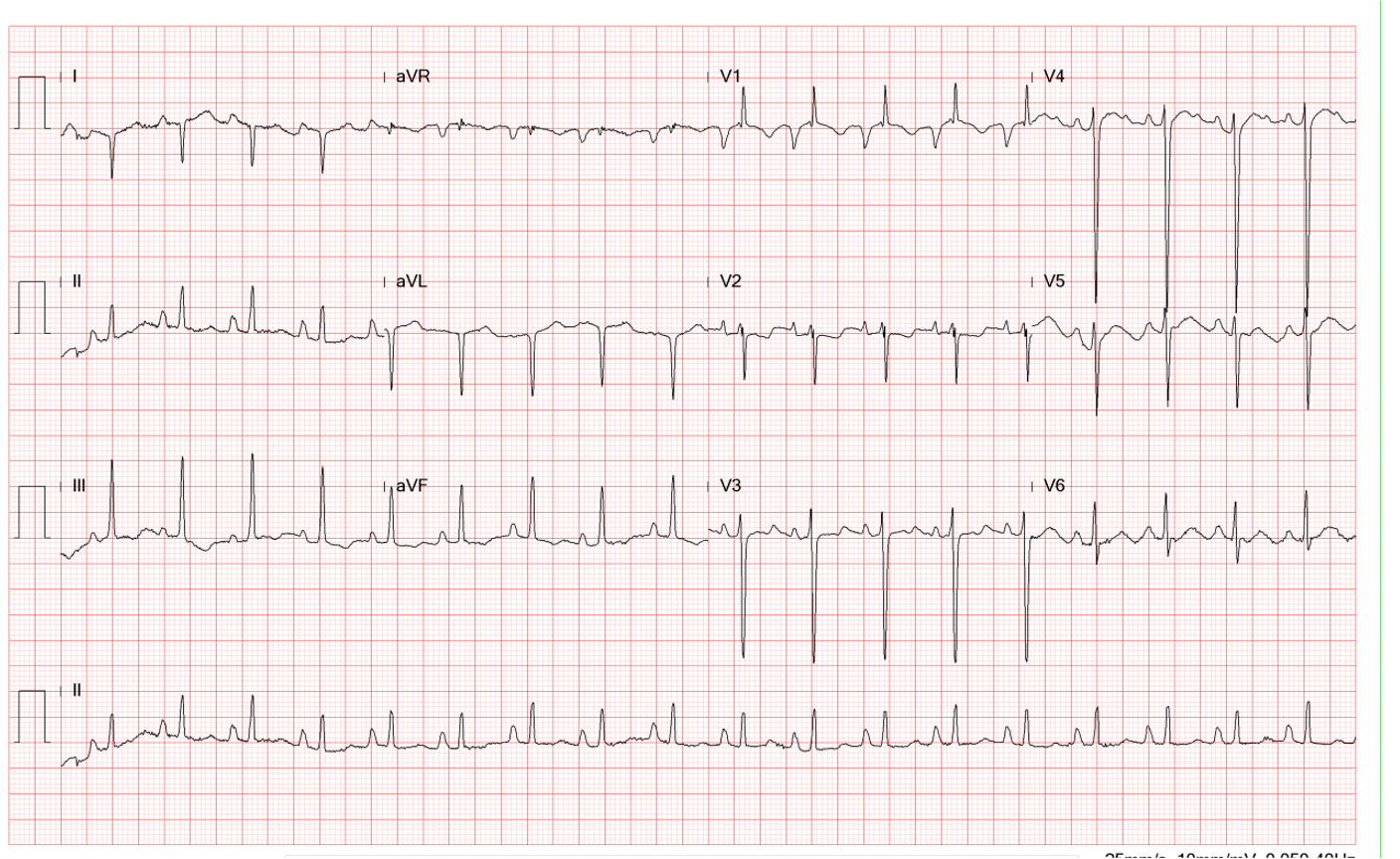
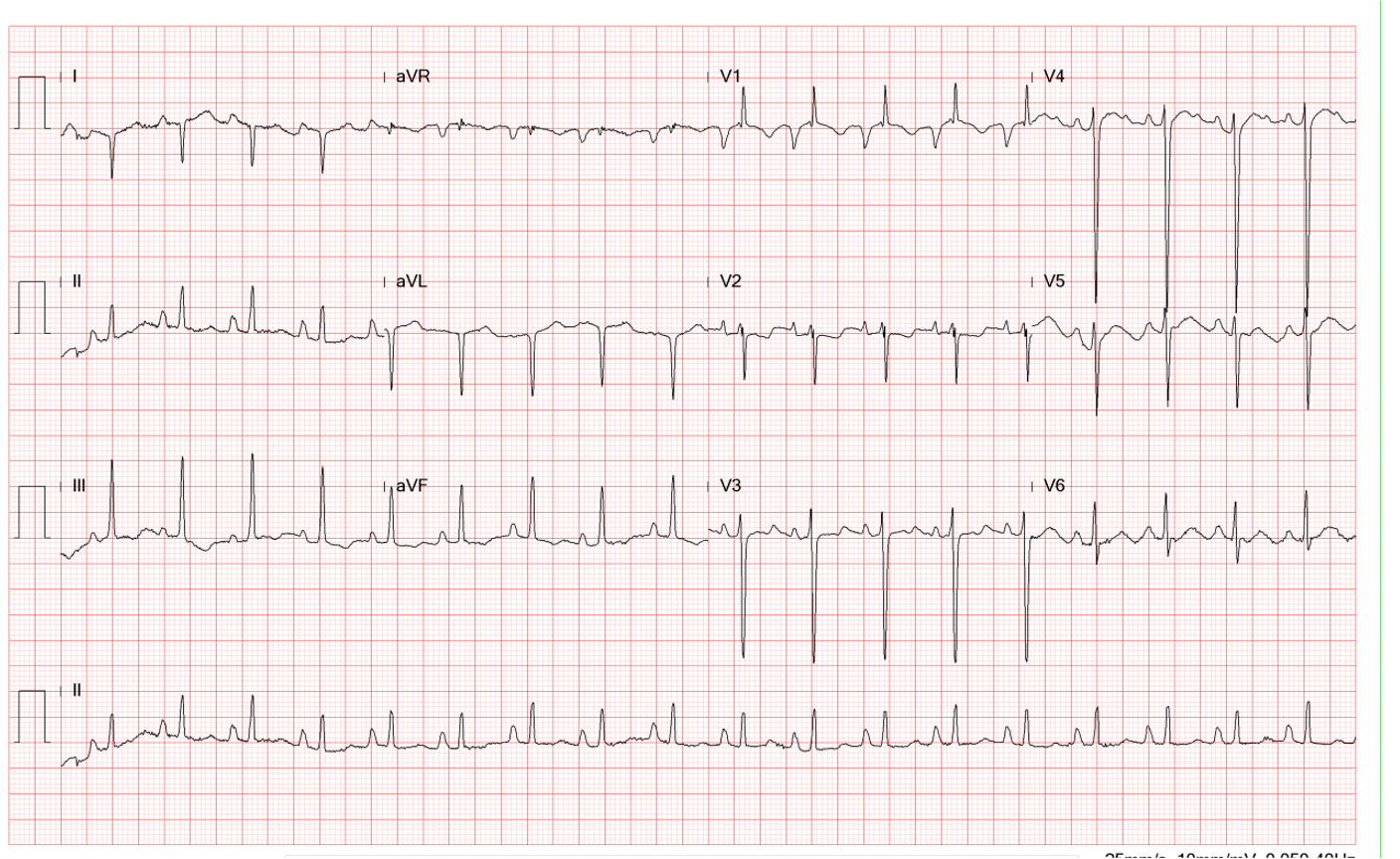
Sinus tachycardia at 118/min
Diffuse low voltage
S1Q3 pattern with left AD (-45°) suggestive of LAHB
IVCD (fractionated QRS, QRSd: 164 msec) with qR in V1 and complete RBBB pattern suggestive of RVH
Q in II, III, and aVF, and V2-V4 with ST elevation in V2-V5 c/w inferior and anterior MI of undetermined age
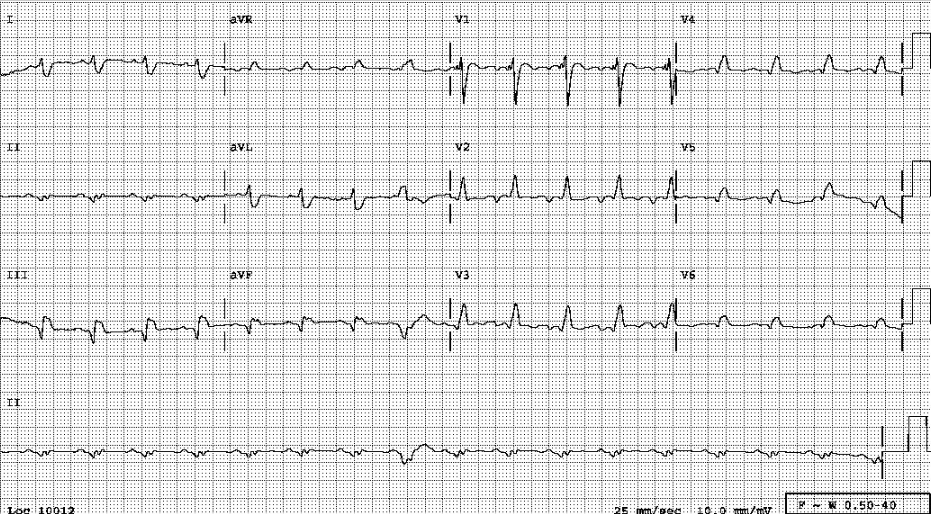
Right-sided ECG showing no ST elevation over V4R.

Cardiomegaly (r/o pericardial effusion)
LA enlargement
Elevation of right hemidiaphragm
Blurring of both CP angles (pleural effusion)
Prominence of minor fissure alongside generalized increase in bilateral lung markings c/w HF
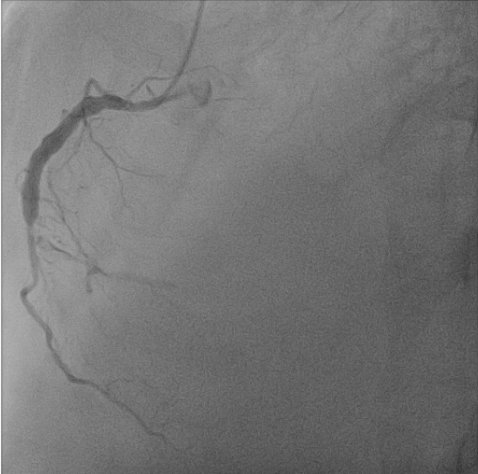
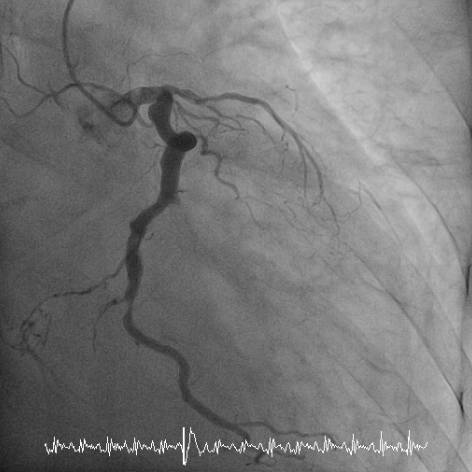
LAD-total occlusion; LCx-distal 70% stenosis; LCx-OM1 total occlusion; RCA-middle total occlusion; Collateral circulation: LCx collateral to LAD and RCA
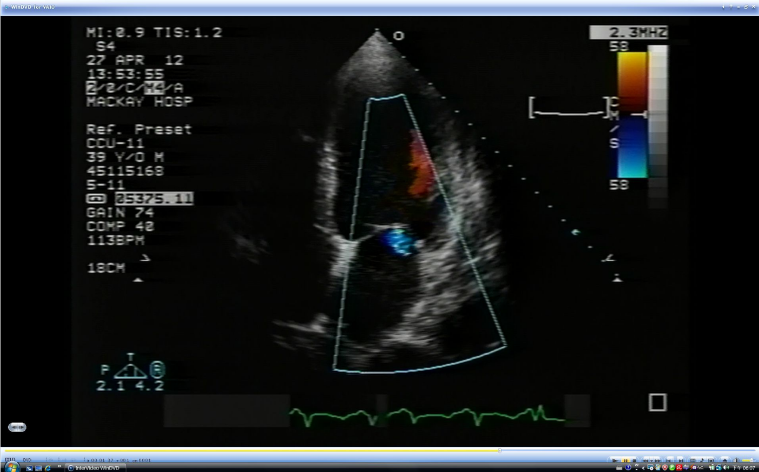
Marked LV enlargement
Severe global LV hypokinesis with regional wall motion
abnormalities in anteroseptal, apical, and inferior segments
Mitral inflow: E/A ratio >1 (Prolonged isovolumic relaxation time).
Moderate MR and severe TR
This ECG is complicated as the findings are consistent with severe atherosclerotic CHD with MI (age undetermined) or extensive cardiomyopathy.
First, besides obesity, the differential diagnosis for diffuse low voltage should also consider pericardial effusion, extensive cardiomyopathy, and severe atherosclerotic CHD with MI. Second, inferior MI renders the QRS axis shift to the left. Still, an additional LAHB, which can cause left axis deviation, is likely to further push the axis to the indeterminate quarter (-135o). Vectorcardiographically (not done), an inferior MI alone shows a clockwise rotation, whereas an inferior MI plus LAHB exhibits a counterclockwise rotation on the frontal plane. Third, with the right BBB pattern (broad R in V1 and wide S in I, aVL, and V5-V6), the so-called “bi-fascicular block” (right BBB plus LAHB) might be present. Nonetheless, the right BBB pattern with or without LAHB in anterior MI (Q in V2-V4) usually indicates a proximal LAD lesion in patients with CHD. Fourth, the qR pattern in V1 suggests RVH. However, the extensive MI, the low voltage, and the left axis have hampered the recognition of RV and LV enlargement.
Of note, unless there is a preexisting cardiac enlargement (e.g., hypertensive cardiomyopathy), cardiomegaly is generally not observed in patients with the first episode of acute MI, even when HF complicates the clinical presentation. This patient had symptoms of HF without chest pain/tightness, which started ten days before admission, and the presence of marked cardiomegaly signaled the chronicity of his cardiac disease. Under the circumstance, the care team reasonably decided to defer immediate coronary angiography aiming at primary PCI despite a slight increase in the cardiac enzyme (CK-MB 1.9 [N <5.0] ng/mL; Tn-I 0.95-0.76 [N <0.12] ng/mL).*
The coronary angiographic findings confirmed extensive triple vessel disease with total occlusion of LAD. The care team advised the patient to undergo complete revascularization with CABG. Before CABG, the patient should have a thallium-persantin exercise scan or MRI imaging to assess the extent of active myocardial ischemia. Furthermore, this 30-year-old patient has premature atherosclerotic CHD (< 55 years for men; < 60 years for women). Most of these patients (75-85%) with premature atherosclerotic CHD have hyperlipidemia. If proven true, the patient and his family (positive family history), including off-springs, should consult a specialist for further medical management to prevent or avert its progression.
*After MI, generally, CK-MB stays elevated for 1-2 days while troponin stays elevated for 1-2 weeks.
Keywords:
bi-fascicular block, premature atherosclerotic coronary heart disease (CHD), primary percutaneous coronary intervention (PCI), thallium-persantin exercise scan
UpTodate:
Primary percutaneous coronary intervention in acute ST elevation myocardial infarction: Determinants of outcome
Coronary artery bypass graft surgery after acute ST
elevation myocardial infarction
HDL-cholesterol: Clinical aspects of abnormal values
Inherited disorders of LDL-cholesterol metabolism
A 56-year-old man came to the Emergency Department because of worsening dyspnea with a productive cough for the past two weeks. Notably, he smoked one

An 83-year-old woman was transferred to Emergency Department (ED) from a local hospital because of a marked deterioration of general status while being treated with
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.