Case 10
A 43-year-old woman, s/p mitral valve (MV) replacement (Bjork-Sheily) for mitral stenosis (MS) associated with rheumatic heart disease 18 years ago, was admitted with worsening
An 84-year-old man with a known history of hypertension, COPD, diabetes, Parkinsonism, and old CVA (putamen infarction)* was noted to be delirious after five days of having reduced appetite and general weakness. A brain CT done at the neurology clinic revealed no significant abnormality. Later, he complained of chest pain and developed intermittent low-grade fever alongside cold sweats but no cough, dysuria, diarrhea, or SOB. At the Emergency Department, he appeared chronically ill. BP measured 117/59 mmHg and BT/PR/RR 35.1C, 100/min (irregular), and 17/min, respectively. Despite basilar crackles in both lungs, there were no signs of heart failure (HF). ECG showed AF with an average ventricular rate of 117/min. Hb was 12.2 gm%, WBC 6890, Plt 144k, SGOT 47 U/L, SGPT 34 U/L, Na 134 mEq/L, K 3.4 mEq/L, BUN 33.7 mg/dL, Cr 1.5 mg/dL, CKMB 4.4 ng/mL, troponin I < 0.05 ng/mL and CRP 9.31 (N <3) mg/dL. Chest X-rays revealed possible RML, LLL pneumonia, and slight cardiomegaly with LA enlargement. After blood samples were drawn for culture, the care team started IV fluid and antibiotics with cefazoline and metronidazole. The following day, the patient became highly uncomfortable; the skin was cold and clammy. BP measured 83/53 mmHg and BT/PR/RR 38.1ºC, 80/min, and 20/min, respectively. ECG exhibited sinus rhythm at 79/min; there was ST-segment (concave) elevation in limb and precordial leads (II, III, aVF, V4-V6), with J point depression in aVR suggesting epicardial injury (e.g., acute pericarditis). Repeated Hb was 11.3 gm%, WBC 13860 (Band 15%) Plt 93k, CKMB 3.7 ng/mL, troponin I < 0.05 ng/mL, lactate 6.21 (N 0. 5 to 2. 2) mmol/L, procalcitonin** 20.54 (N <0.1 ) ng/mL. The care team quickly infused normal saline 1500ml and raised BP to 120/77mmHg with levophede drip (6.5mcg/min). Under the suspicion of septic shock vs. “cardiac tamponade” due to “aortic dissection,” the care team obtained a chest CT scan with contrast. It revealed no aortic dissection, but there was cardiomegaly with pericardial effusion. Pericardiocentesis removed 350ml yellow turbid viscous liquid (pus) with a Sp.gr of 1.037, protein-positive, containing RBC 1520 /cumm and WBC 8560 (neutrophil 99 %) /cumm. The hemodynamics became stable even after tapering off the levophed drip. The specialist felt the additional finding of pericholecystic fluid collection on the CT scan was a benign condition. Subsequent blood cultures grew positive for salmonella group D, as did the pericardial fluid. A surgical pericardiotomy*** was then performed to prevent reaccumulating pericardial effusion. To treat Salmonella sepsis, the care team used ceftriaxone, a 3rd generation cephalosporin, based on sensitivity testing to suppress salmonella sepsis with purulent pericarditis. Lastly, echocardiography showed preserved LV contractility (EF:65%), small residual pericardial effusion, and no abnormal regional wall motion. In retrospect, the only significant history likely to be the source of salmonella infection was that he had “sushi” (Japanese raw fish meal) for supper a few days before he became sick.
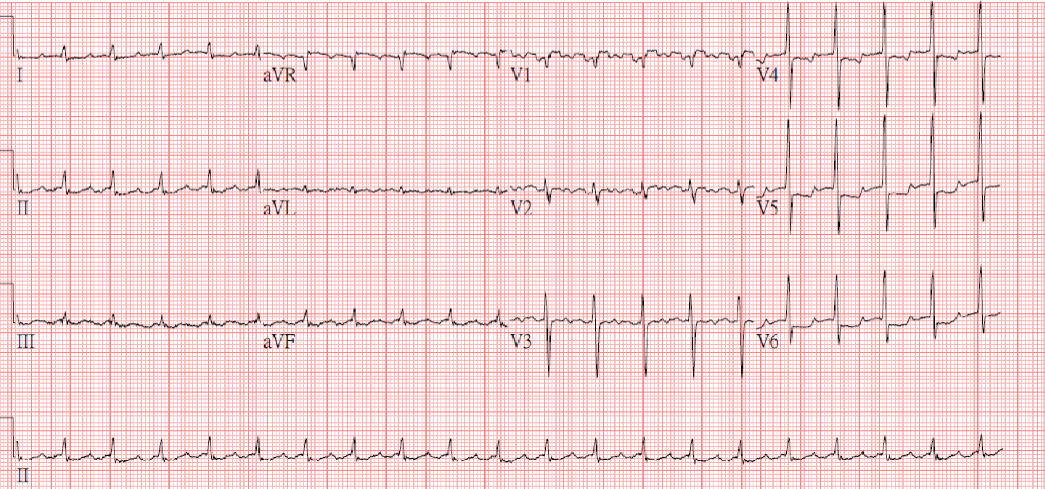
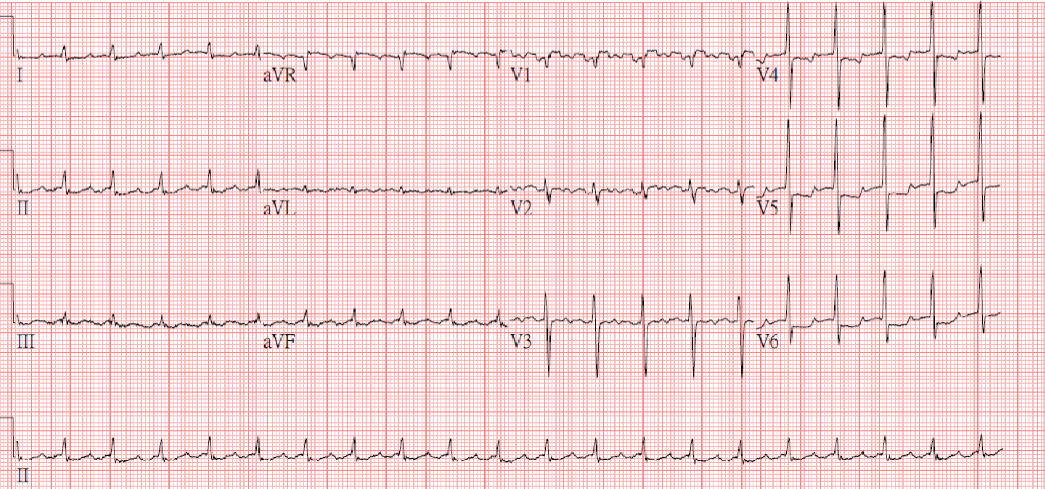
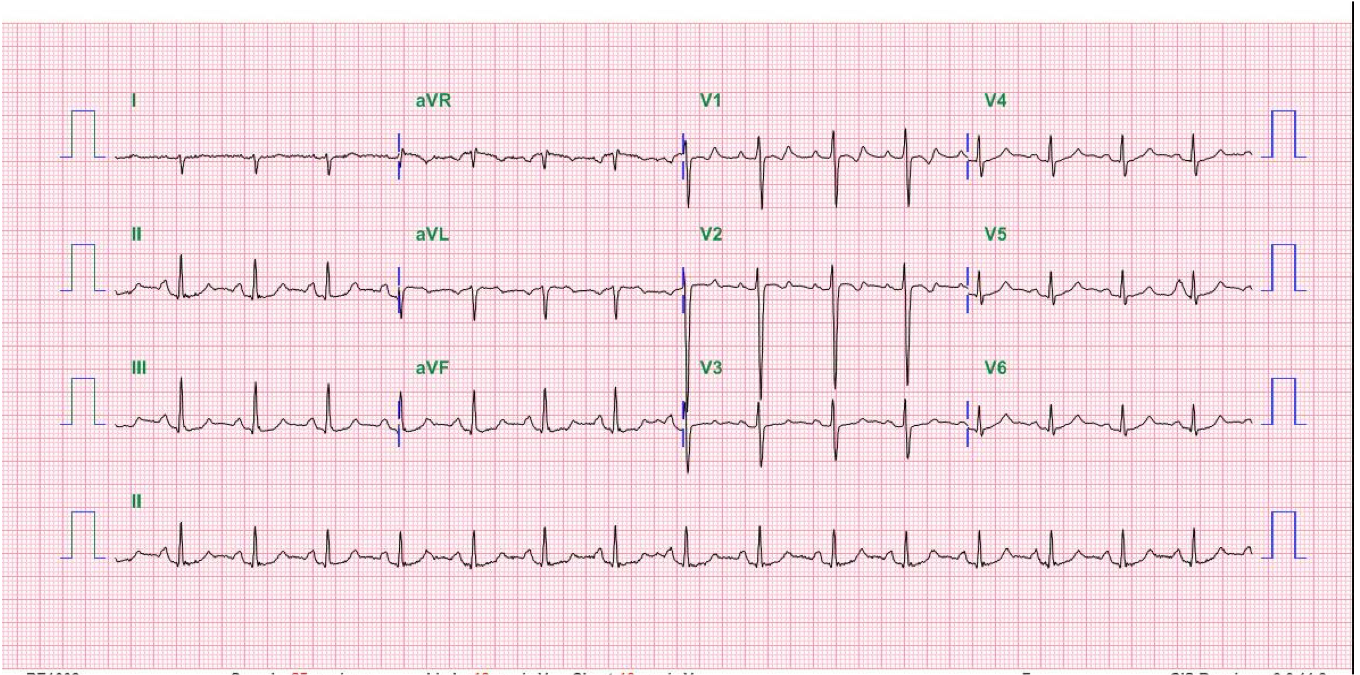
AF with an average ventricular rate of 84/min
Low voltage in limb leads and slow progression of R waves in precordial leads suggestive of COPD
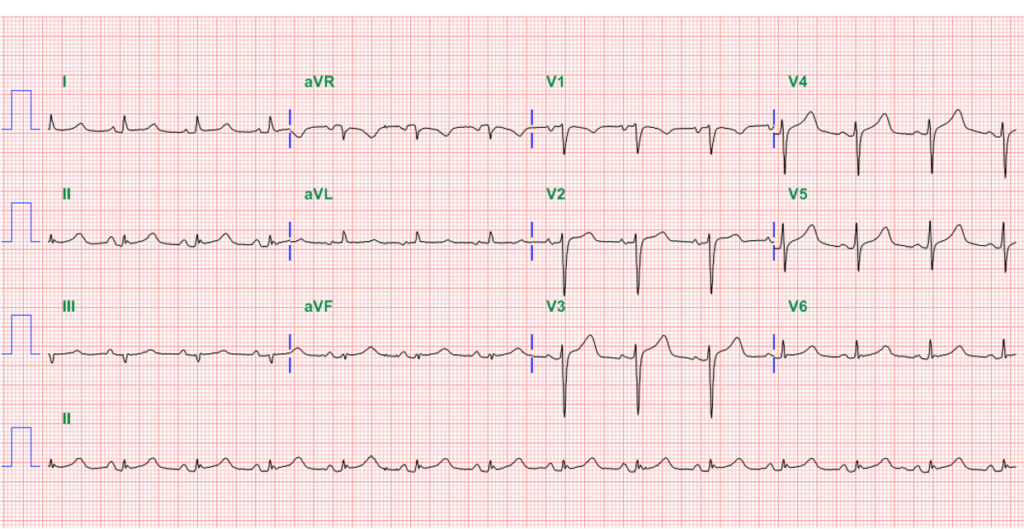
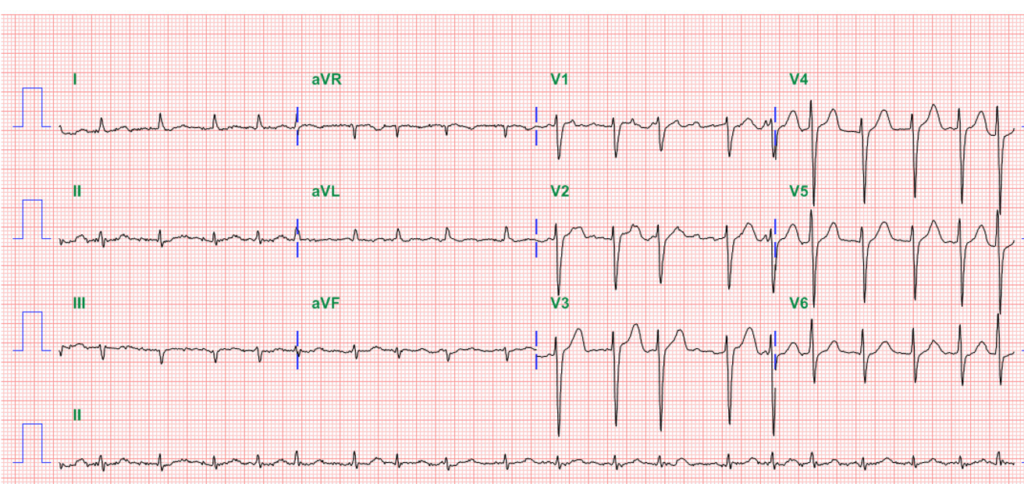
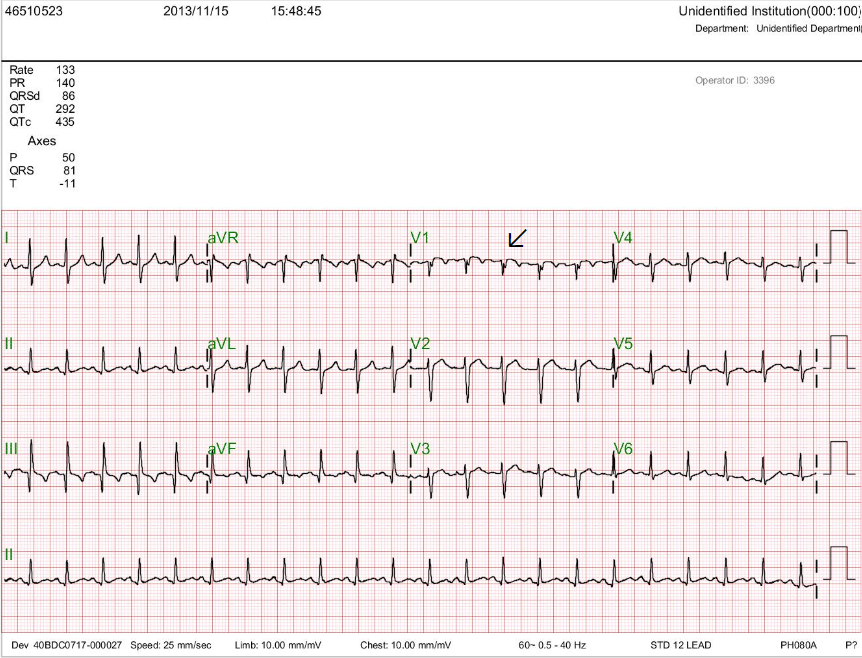
Sinus rhythm at 77/min
Low voltage in limb leads
Concave ST-segment elevation in limb and precordial leads II, III, aVF, V4-V6, and reciprocal J
Point depression (ST-segment depression) in aVR, suggesting acute pericarditis.
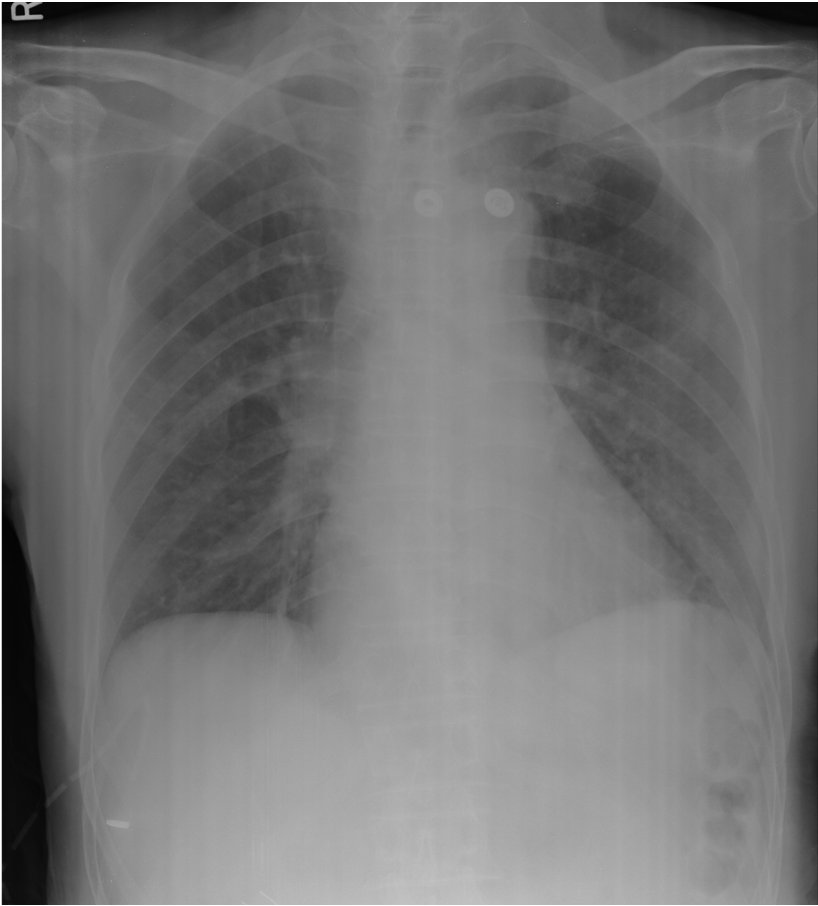
Slight cardiomegaly (AP view).
LA enlargement (i.e., widened carina coupled with a slightly bulged cardiac border below the left PA).
Infiltrates at both lower lung fields (RML and LLL) suggestive of pneumonia
No pulmonary congestion

No evidence of aortic dissection
Cardiomegaly with pericardial effusion
Subsegmental atelectasis in both lower lobes
bilateral pleural effusion.
Bilateral calcific lymph nodes noted.
Clustered lymph nodes in the mediastinum at the aortic arch.
Spondylosis of T-L spine.
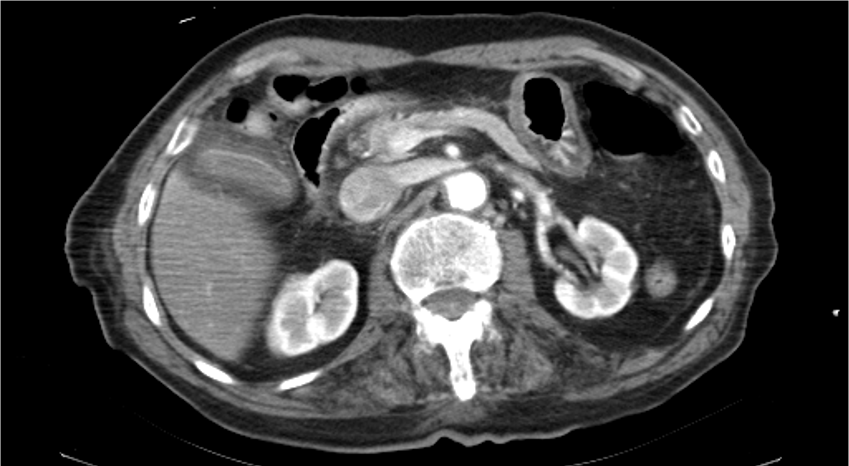
Pericholecystic fluid collection.
In the present case, COPD and pericardial effusion contribute to low voltage. When first seen, it is very likely this patient with a change in mental status (becoming delirious) has already had a salmonella infection. Unfortunately, in severe bacterial infection, elderly patients (e.g., octogenarians) may have delayed responses in body temperature and white blood cell counts- afebrile and absence of leukocytosis (WBC 6890). Notably, the ECG findings of acute pericarditis appear with worsening clinical symptomatology with impending shock (BP dropped from 117/59 to 83/53 mmHg). A chest CT scan with contrast instead of echocardiography is appropriate because aortic dissection with cardiac tamponade is of primary concern.
The characteristic ECG findings in pericarditis include diffuse ST segment elevation in multiple leads, PR segment depression, and PR segment elevation and reciprocal J point or ST segment depression in aVR. The ST segment elevation is typically concave upward, giving it a “saddle-shaped” appearance. This contrasts the ST segment elevation seen in myocardial infarction, which generally is convex upward. It is important to note that concave ST segment elevation alone cannot diagnose pericarditis. Clinical history, physical examination findings, and other diagnostic tests, such as echocardiography and cardiac biomarkers, are also crucial to accurately diagnosing. Clinicians should be aware of the characteristic ECG findings in pericarditis and consider them in the differential diagnosis of patients presenting with chest pain and other symptoms suggestive of pericardial inflammation.
Cardiac tamponade is a medical emergency characterized by the accumulation of fluid or blood in the pericardial sac, leading to heart compression. Common causes of cardiac tamponade include trauma, such as a penetrating injury to the chest, and medical conditions like pericarditis, malignancy, and aortic dissection. The classic clinical presentation includes Beck’s triad, which consists of hypotension, muffled heart sounds, and jugular venous distention. Other signs and symptoms may include dyspnea, tachycardia, pulsus paradoxus, and signs of systemic hypoperfusion. Prompt diagnosis and management are crucial. Diagnostic modalities such as echocardiography and cardiac catheterization can help confirm the diagnosis and assess the severity of tamponade.
The primary treatment for cardiac tamponade is pericardiocentesis. In some cases, surgical intervention may be necessary to relieve the tamponade and repair any underlying causes. Clinicians must promptly recognize the signs and symptoms of cardiac tamponade and initiate appropriate interventions. Early intervention can significantly improve patient outcomes and prevent further complications.
Infectious pericarditis refers to inflammation of the pericardium, which can be bacterial, viral, fungal, or parasitic. Infectious pericarditis can lead to the accumulation of fluid in the pericardial space, known as pericardial effusion. On the other hand, purulent pericarditis specifically refers to infectious pericarditis characterized by pus in the pericardial space. It is usually caused by a bacterial infection, Staphylococcus aureus or Streptococcus pneumoniae. Purulent pericarditis is a severe condition that requires prompt diagnosis and treatment, as it can lead to complications such as cardiac tamponade, sepsis, and death. Thus, infectious pericarditis is a broad term encompassing all types of inflammation caused by an infection, and purulent pericarditis refers explicitly to contagious pericarditis characterized by pus.
Salmonella group D includes Salmonella enterica serotype Enteritidis and Salmonella enterica serotype Typhimurium. S. Typhi is the most frequent causative agent of enteric fever. Salmonella group D is a gram-negative, rod-shaped bacterium that can cause enteric fever (paratyphoid fever). Paratyphoid fever is similar to typhoid fever but is generally milder in severity. Salmonella group D is primarily transmitted through contaminated food or water consumption. The bacteria can invade the intestinal lining and spread to other organs, leading to symptoms such as high fever, abdominal pain, diarrhea, and general malaise. In severe cases, complications such as intestinal perforation or bloodstream infection can occur. Diagnosis of Salmonella group D infection is typically done through stool or blood culture to isolate and identify the bacteria. Treatment involves using antibiotics to eliminate the infection and supportive care to manage symptoms and prevent dehydration. Preventing Salmonella group D infection involves practicing good hygiene, such as thorough handwashing, proper food handling and preparation, and avoiding consuming contaminated food or water. Vaccines are also available for specific serotypes of Salmonella, but currently, there is no particular vaccine for Salmonella group D.
Treating Salmonella sepsis involves a combination of antibiotics and supportive care. Antibiotics are used to target the specific strain of Salmonella causing the infection. Commonly used antibiotics include fluoroquinolones, third-generation cephalosporins, and extended-spectrum penicillins. The antibiotic choice depends on the strain’s susceptibility and the patient’s clinical condition. Supportive care is also essential in the management of salmonella sepsis. This includes maintaining adequate hydration and electrolyte balance and monitoring and managing any complications that may arise.
*Putamen infarction refers to the occurrence of an ischemic stroke in the putamen region of the brain. The putamen is a part of the basal ganglia, which plays a crucial role in motor control and coordination. Infarction in this area can lead to various motor and cognitive impairments, depending on the extent and location of the damage. Common symptoms of putamen infarction include weakness or paralysis on one side of the body, difficulty with coordination and balance, and changes in speech and language.
** Procalcitonin is a protein the body produces in response to bacterial infections. A procalcitonin test measures the level of procalcitonin in the blood and is used to diagnose sepsis.
***Pericardiotomy is a surgical procedure involving an incision in the pericardium, the sac-like structure surrounding the heart, to drain excess fluid or blood accumulated around the heart. On the other hand, pericardiectomy is a surgical procedure that involves removing part or all of the pericardium. It is performed to treat constrictive pericarditis, a condition in which the pericardium becomes thickened and stiff, making it difficult for the heart to function.
Keywords:
cardiac tamponade, purulent pericarditis,Salmonella infection, septic shock
UpToDate:
Cardiac tamponade
Nontyphoidal Salmonella bacteremia
Purulent pericarditis
A 43-year-old woman, s/p mitral valve (MV) replacement (Bjork-Sheily) for mitral stenosis (MS) associated with rheumatic heart disease 18 years ago, was admitted with worsening
A 20-year-old man awakened from sleep with severe chest tightness and shortness of breath (SOB). Simultaneously, he felt dizzy and nauseous and fainted with crutches
A 52-year-old man was admitted because of progressive dyspnea on exertion for one week. In the past, he had chronic obstructive pulmonary disease (COPD), alcoholic
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.