Case 11
A 38-year-old man was admitted because of having abdominal fullness associated with progressive SOB (PND and orthopnea) for ten days. He denied having abdominal pain,
A 65-year-old man was brought in with progressive edema of the left arm below the elbow level for two weeks. It was not “red and hot” but painful. In addition, he noted leg edema, PND, and increasing SOB on exertion.
He denied fever, chills, and chest pain. PMH was significant for DM and chronic HF associated with atherosclerotic CHD (s/p MI and PTCA 10 years ago).
At ED, he appeared obese and chronically ill in moderate respiratory distress (afebrile, PR 95 /min, RR 20/min, and BP 135/63 mmHg). Physical findings showed biventricular HF (JVD with JVP 10cm H2O, bilateral crackles, percussion dullness at the lung base, and PMI displaced to the left. S1 widely split, a Gr 3/6 TR murmur increased in intensity with inspiration and bilateral pitting leg edema). Pertinent laboratory data included HbA1c 12.4 %Hb, Hb 13.2 g/dL, Ht 40%, WBC 14,320 /uL, Na 139 mEq/L, K 3.1 mEq/L, and D-dimer 783.75 ng/mL. Echocardiography showed dilated RA, LA, and RV, global LV hypokinesis (LV EF 25%), moderate MR and severe TR, downward displacement of septal and posterior leaflets of the tricuspid valve with a large anterior leaflet which exhibited delayed closure relative to the mitral valve accounting for widely split S1 (sail sound)*, moderate PAH, and engorgement of inferior vena cava.
Of note, sonography of the left cephalic vein disclosed venous thrombosis at the distal end. Anticoagulation therapy was then instituted, along with a surgical consultation.
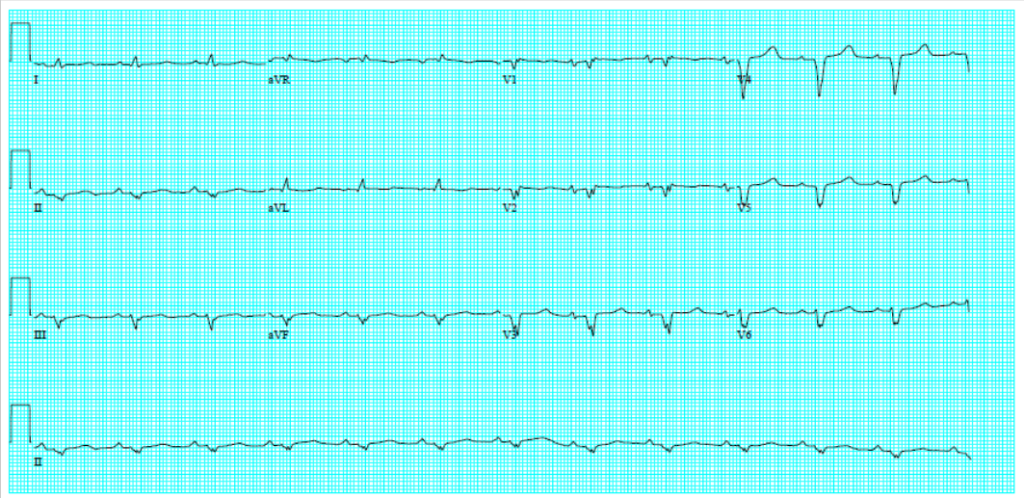
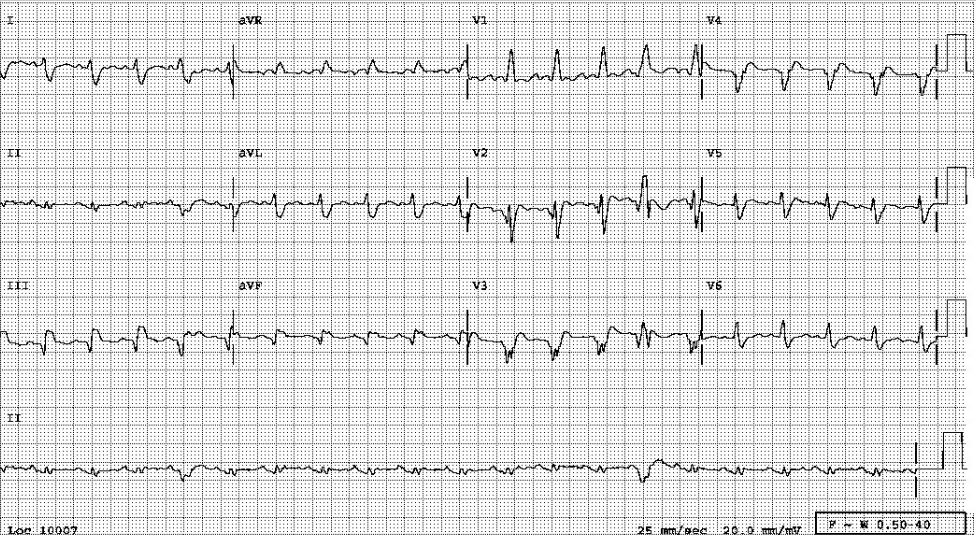
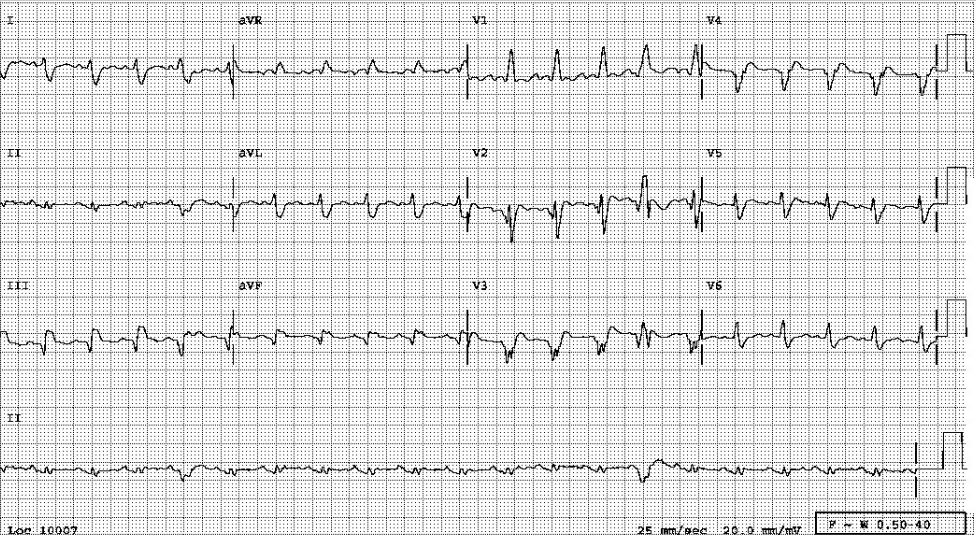
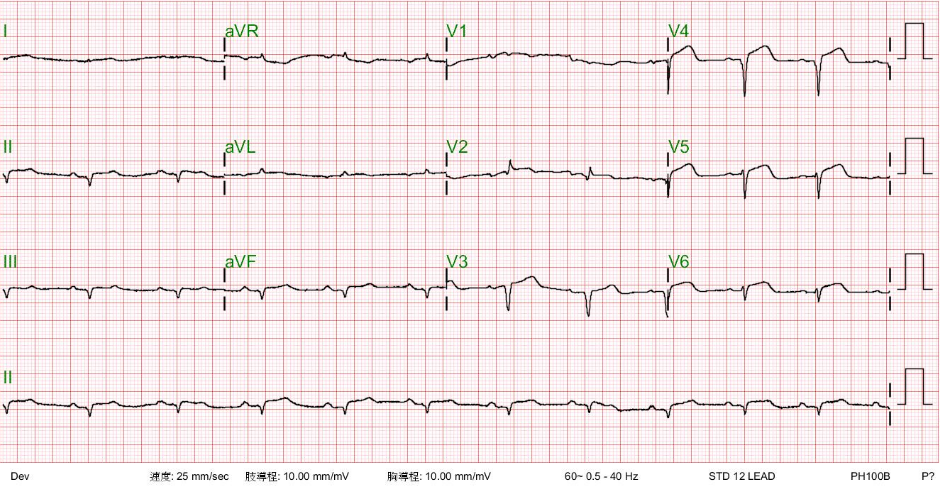
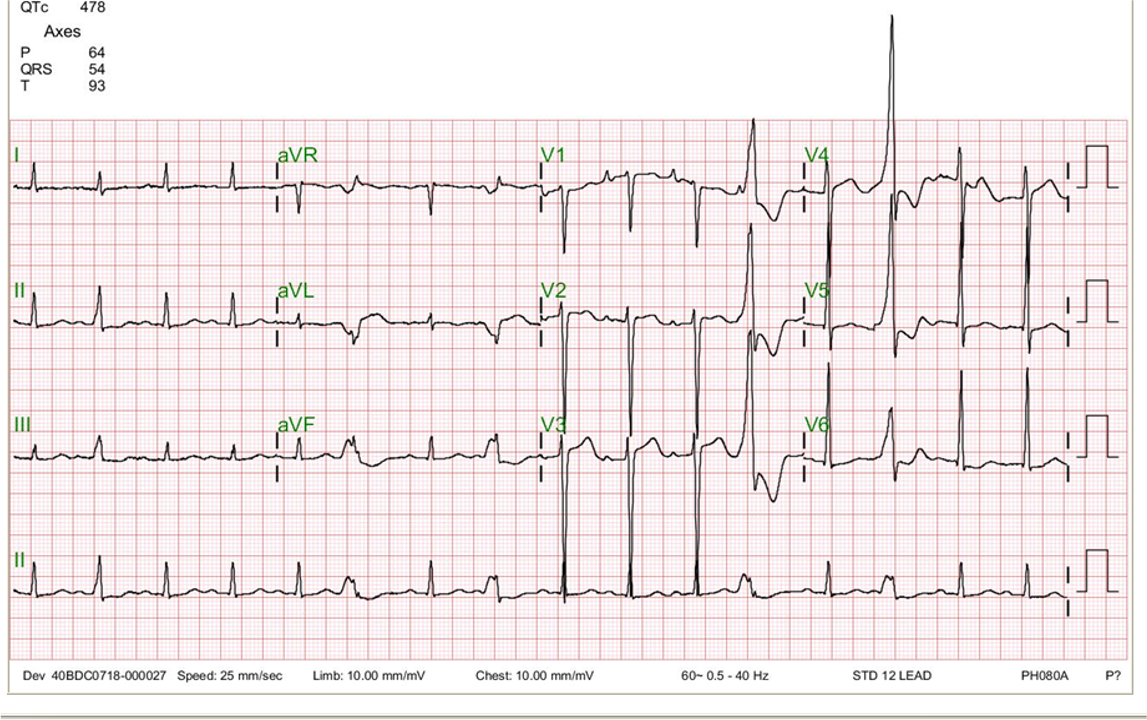
Sinus rhythm at 60/min.
Diffuse low voltage
Left AD (-90°)
IVCD (fractionated, QRSd 128 msec) with r in V1 and s in I, a tendency toward incomplete RBBB pattern
QS in V1-V5 and small r in II, III, and aVF c/w anterolateral MI and inferior MI, respectively, of undetermined age

LVH
LA and RA enlargement
Pulmonary congestion with bilateral pleural effusion, R > L
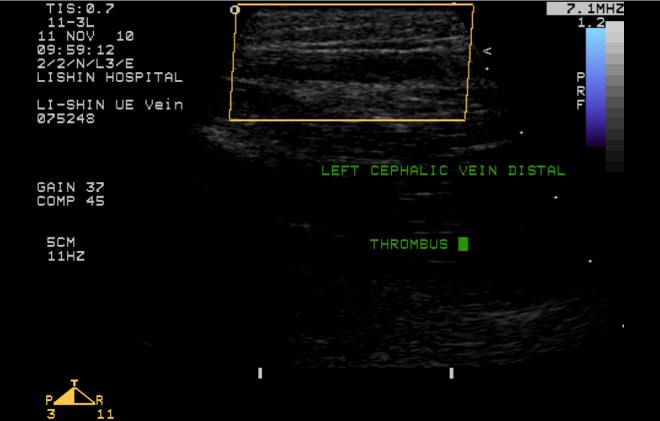
Venous thrombosis
The cause of diffuse low voltage in all ECG leads is multifactorial. In the present case, loss of R wave from previous MIs and marked RA enlargement due to Ebstein’s anomaly are contributing factors. However, other causative possibilities, such as pericardial effusion, COPD, and relative obesity, should also be entertained.
Considering the left cephalic vein thrombosis, Virchow’s triad depicts the propensity for the occurrence of thrombosis:
The clinical conditions favoring venous thrombosis in the present case include immobility and chronic HF. Immediate treatment with intravenous heparin is indicated to dissolve the thrombosis, followed by long-term anticoagulation (e.g., apixaban or rivaroxaban) after bleeding risk stratification.
About biventricular HF with JVD and bilateral leg edema, CHD with prior MI and Ebstein’s anomaly are additive factors. Ebstein’s anomaly is characterized by an apical displacement of both the septal and posterior TV leaflets (exceeding 20 mm in adults). Consequently, the right heart consists of three components: true RA, the functional RV, and an intervening zone that is anatomically RV structure but functions as RA (atrialized RV). TR is usually moderate to severe.
Ebstein’s anomaly can have variable severity and protean clinical presentation. Aside from wide S1 split with sail sound* and severe TR, ECG and chest X-ray findings are not typical in the present case because of secondary cardiomyopathy caused by DM and atherosclerotic CHD with prior MI. Ebstein’s anomaly is often complicated by an ASD (left to right shunt) and accessory AV bypass tracts (WPW syndrome). In light of significant co-morbidity, the risk of surgical repair/replacement of the tricuspid valve is relatively high. A congenital cardiovascular specialist should be included in the consultation.
*The Sail Sound in Ebstein’s anomaly: Phonocardiographically, the closing of the tricuspid valve has two components. It occurs with a first low-amplitude component (T1), originating at the tip of the tricuspid leaflets, and a second high-amplitude component (T2, ‘sail sound’), arising from the body of the tricuspid leaflets. Thus, the ‘sail sound’ is a complex mosaic closing sound that includes “a sudden stopping sound after the anterior and other tricuspid leaflets balloon out at systole.”
Keywords:
diffuse low QRS voltage, Ebstein’s anomaly, venous thrombosis, Virchow’s triad
UpToDate:
Overview of the causes of venous thrombosis
Overview of the treatment of proximal and distal lower extremity deep vein thrombosis (DVT)
Management and prognosis of Ebstein anomaly
Oki et al. The ”sail sound” and tricuspid regurgitation in Ebstein’s anomaly: the value of echocardiography in evaluating their mechanisms. J Heart Valve Disease 6:189-192,1997
A 38-year-old man was admitted because of having abdominal fullness associated with progressive SOB (PND and orthopnea) for ten days. He denied having abdominal pain,
This 69-year-old man had been in good health until two days before admission when he returned from a beach. He experienced general weakness with chest
This 92-year-old man complained of progressive dyspnea with PND, productive cough with whitish sputum, and bilateral leg edema for the past few weeks. He was
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.