
Case 3
A 62-year-old man was brought to Emergency Department for severe chest tightness of sudden onset, lasting 30 min. He had experienced episodes of chest tightness
An 83-year-old woman was transferred to Emergency Department (ED) from a local hospital because of a marked deterioration of general status while being treated with antibiotics for pneumonia for one week. Specifically, she had a persistent high fever despite intensive care, and she developed diarrhea, seizure, mental confusion (negative brain CT), and heart failure (HF), culminating in cardiogenic shock (LV EF 15%). ECG then also showed changes suggesting acute anteroseptal STEMI. PMH was only significant for long-standing hypertension. On arrival, she was febrile (39.7°C), intubated, unconscious, and hypotensive (BP 75/50 mmHg under levophed infusion). PR was 150/min, RR 20/min. The skin was dry, and the turgor was poor. Extremities were cold but not cyanotic. There was no JVD. The chest was kyphotic, and the lungs were clear (after diuresis). PMI was displaced to the left. Heart sounds were distant, and no significant murmurs were heard. The abdomen was distended with reduced bowel sounds. Multiorgan dysfunction was noted (Hb 15.3 g/dL, WBC 22,110 /uL, hsCRP 0.93, BUN 67 mg/dL, Cr. 1.8 mg/dL, Na 154 mEq/L, K 2.8 mEq/L, Ca 7.4 mg/dL, ALT 1300 (N 7-55) U/L, total bilirubin 1.10 (N 0.1-1.2) mg/dL, Alk-P 50 (N 40-129) U/L, INR 1.8, CPK-MB 2.9 (N: <5.4) ng/mL, Tn-I 5.9 (N: <0.5) ng/mL, and ABG: pH 7.53 (N 7.35-7.45), PO2 255 (N 75-100) (FIO2 100%) mmHg, CO2 20 (N 32-45) mmHg, HCO3 16.7 (N 20-26) mmol/L, BE -4.0 (N -2.0 – +2.0) mmol/L. Blood, urine, and spinal fluid cultures were negative. Notably, subsequent cardiac catheterization with coronary angiography showed no significant lesions in all coronary arteries; there was LV enlargement with MR. EF was 33.2%, CO 3.08 (N 3.1-6.4) L/min and Cl 2.37 (N 2.1-3.2) L/min/m2. While correcting over-diuresis-induced hypovolemia, thyrotoxicosis was suspected. Further laboratory testings unveiled TSH 0.069 [N 0.40-4.0] uIU/mL, Free T4 1.45 [N 0.89-1.76] ug/dL, Cortisol PM: 52.41, anti-TPO Ab: < 10 IU/ml, anti-thyroglobulin Ab: < 20 IU/ml*. Under the impression of a thyroid storm, antithyroid drug therapy, propranolol, and Lugol’s solution were immediately instituted, and her condition gradually improved.
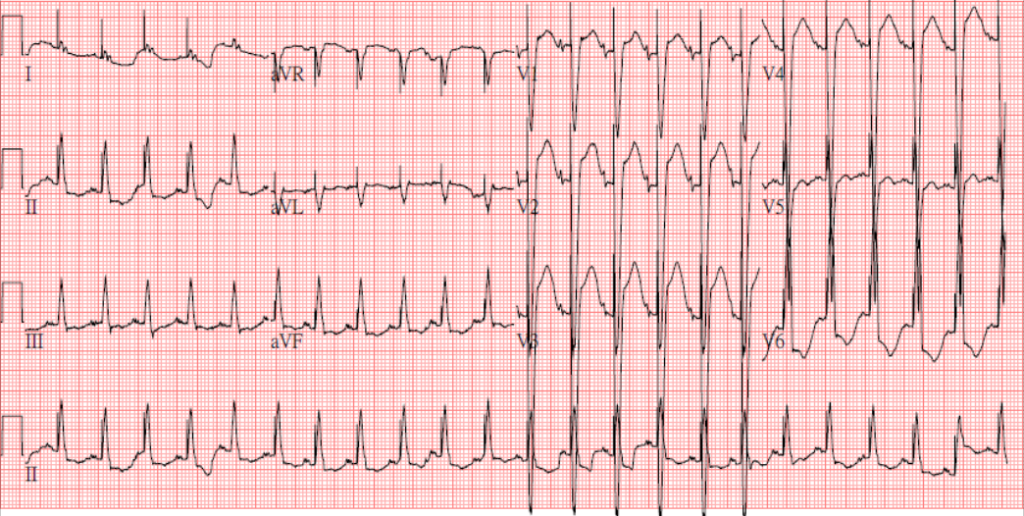
Sinus Tachycardia at 140/min.
LA enlargement
LVH and incomplete LBBB (QRSd 110msec)
ST elevation > 2 mm in V1-V3 and ST depression in V6 suggestive of acute anteroseptal MI
A notable pacing (artifact) spike preceding each QRS complex.
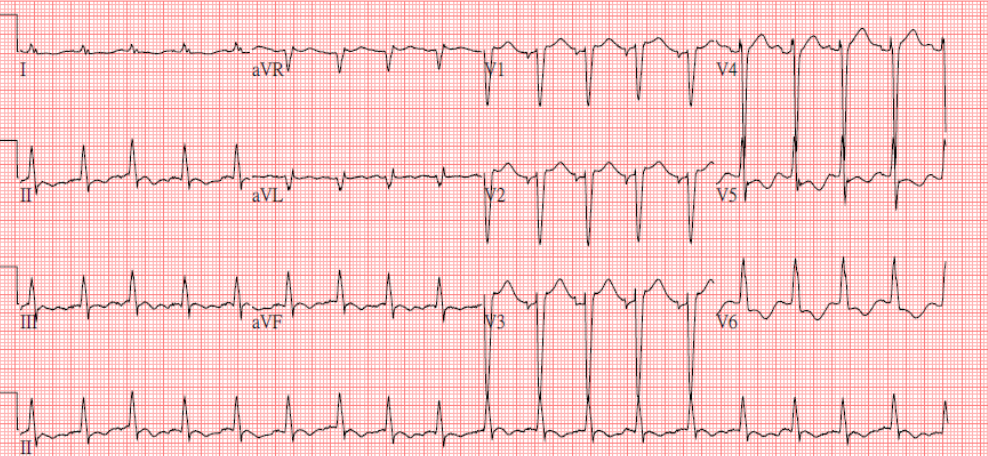
Sinus Tachycardia at 107/min.
LA enlargement
LVH and incomplete LBBB (QRSd 110msec)
Less ST elevation and no pacing spikes compared to the previous tracing

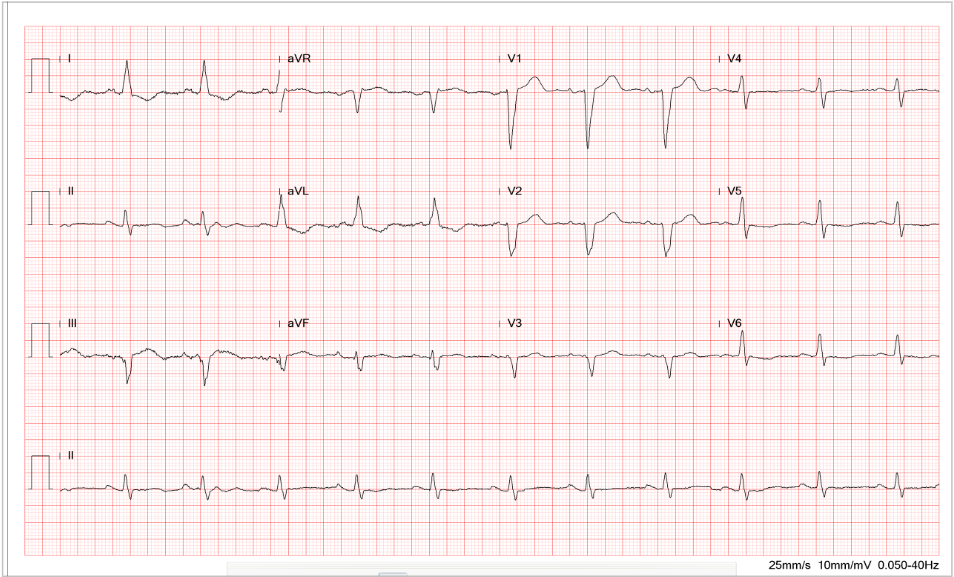
Endotracheal tube in place
Scoliosis
COPD
LVE
Prominent PA suggestive of PH
Dilated colon
With a long-standing history of hypertension, the ECG’s LVH and chest X-ray findings of LV enlargement are likely a form of hypertensive cardiomyopathy. However, the cause of STEMI in the absence of significant coronary lesions remains intriguing. Hyperthyroidism, especially in thyrotoxicosis, can provoke acute MI (STEMI and NSTEMI) (type 2 myocardial infarction)** or cause an acute form of cardiomyopathy (myocardial stunning) without significant coronary heart disease (CHD). In the latter scenario, it has been postulated that diffuse coronary spasm or thrombosis might be the underlying mechanism. Alternatively, it can be likened to stress-induced (Takotsubo) cardiomyopathy relating to the surge of excessive catecholamines or the direct toxic effect of thyroxine on the myocardium.
Since the patient has received neither temporary nor permanent pacemaker implantation, the spike seen with each QRS is presumably an artifact produced by an electrical connection in ED or intensive care unit. It mimics pacing with a QRS-triggered pacemaker (currently obsolete). The spike disappears in subsequent follow-up tracings.
Thyroid storm is an exaggerated form of thyrotoxicosis, commonly presenting with hyperpyrexia (104 to 106°F), agitation, delirium, and severe mental status changes (stupor, come). Its onset is often precipitated by infection (probably pneumonia in this case), pregnancy, surgery, or trauma. Other causes include withdrawal of antithyroid medication, iodine ingestion, amiodarone therapy, etc. Patients with thyroid storm often present with life-threatening symptoms such as hyperpyrexia, altered mentation, and multiorgan dysfunction, e.g., heart (HF, MI, myocardial stunning), liver (fulminant hepatitis), CNS (seizure, coma, encephalopathy), kidney (acute injury), gastrointestinal system (diarrhea, ischemic bowel), lactic acidosis, etc. associated with biochemical evidence of hyperthyroidism (elevation of T4 [free thyroxine] and/or T3 [triiodothyronine] and suppression of TSH [thyroid-stimulating hormone]). However, the magnitude of thyroid hormone changes doesn’t usually correlate with the degree of illness. A thyroid storm is a medical emergency, and recognizing its diverse clinical presentations is challenging. Early diagnosis followed by appropriate treatment is essential for preventing the catastrophic outcomes associated with this condition, i.e., supportive management in the intensive care unit and prompt institution of antithyroid drugs, beta-adrenergic drugs, and corticosteroids can reverse multiorgan dysfunction.
*Anti-TPO Ab (Thyroid Peroxidase Antibodies): Its elevation suggests Hashimoto thyroiditis.
Anti-thyroglobulin Ab: High levels can be seen in Graves disease or overactive thyroid, Hashimoto thyroiditis, thyroid cancer, autoimmune thyroiditis,systemic lupus erythematosus, and Type 1 diabetes.
**Type 2 myocardial infarction: MI caused by a mismatch between oxygen supply and demand with or without CHD rather than that (type 1) with CHD precipitated by atherosclerotic plaque disruption (rupture or erosion).
Keywords:
myocardial stunning, thyroid storm, thyrotoxicosis, type 2 myocardial infarction
UpTodate:
Overview of the clinical manifestations of hyperthyroidism in adults Thyroid storm
Thomas et al. Critical issues in endocrinology. Clin Chest Med. 24:583-606, 2003
Chong et al. Thyroid storm with multiorgan failure. Thyroid 20:333-6, 2010.

A 62-year-old man was brought to Emergency Department for severe chest tightness of sudden onset, lasting 30 min. He had experienced episodes of chest tightness

This 30-year-old woman complained of having had about ten episodes of syncope associated with mild exertion for the past six months.
A 73-year-old woman, s/p ICD implanted for recurrent ventricular tachycardia (VT) associated with dilated cardiomyopathy (DCM) 9 months ago, was admitted after receiving several electrical
If you have further questions or have interesting ECGs that you would like to share with us, please email me.
©Ruey J. Sung, All Rights Reserved. Designed By 青澄設計 Greencle Design.